Going digital to disrupt the addiction epidemic
Modernizing addiction treatment with tech
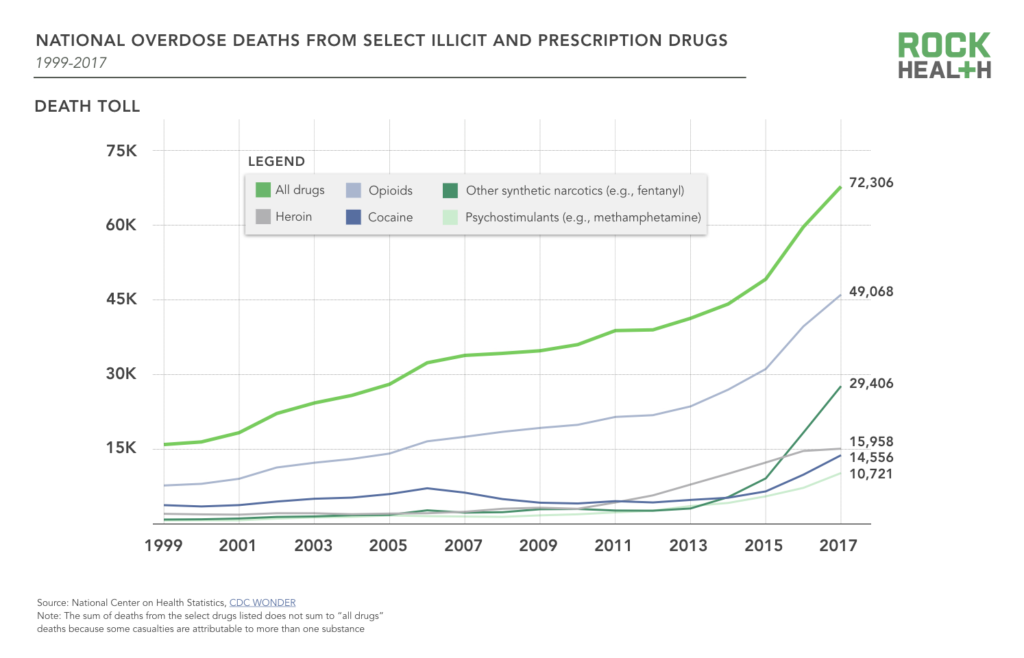
The toll of America’s addiction epidemic continues to dominate headlines—from Instagram becoming a marketplace for advertising illegal drugs to fentanyl’s role in the rise of cocaine deaths. 63.6K people in 2016 died from a drug overdose—a 21% increase from 2015 and three times more people than in 1999.1 This growth is not just from opioid and fentanyl-related mortality spikes—overdose deaths also increased across all types of drugs, among all races, ethnicities, genders, ages, and areas of urbanization. With no groups spared, Americans overwhelmingly believe drug addiction is a problem in their local communities.
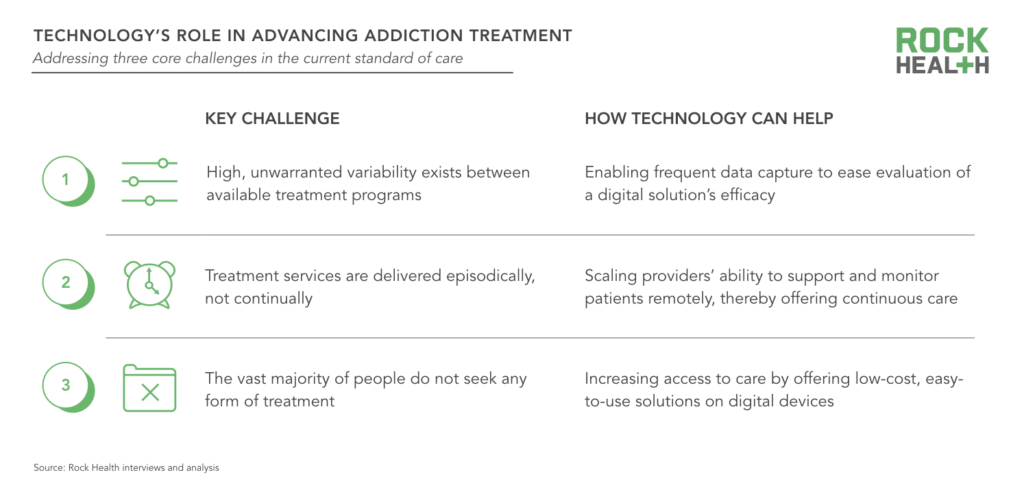
The 20.1M Americans with substance use disorder (SUD)—in addition to millions who do not meet the clinical threshold for diagnosis—stand to benefit from greater access to evidence-based treatment. It’s a long road ahead, but we’re energized by the ways in which entrepreneurs are leveraging technology to address three of the core issues plaguing treatment:
1. High, unwarranted variability exists between available solutions
Not all addiction treatment programs are created equal. In fact, the great majority of people seeking treatment do not receive anything approximating evidence-based care. In the absence of empirically supported programs, 40-60% of individuals receiving treatment for SUD will relapse.
The new technology-centric solutions we’ve reviewed provide evidence-based programs grounded in foundational research studies of effective interventions. These digital solutions allow for more frequent data capture regarding engagement with and adherence to a program, which enables evaluation of a solution’s outcomes and modification of the program over time. With app-based solutions on the rise, collected data has the potential to be more robust than ever before.
2. Services are delivered episodically, not continually
Addiction care tends to be delivered in fragmented episodes with intensive treatment provided for a short period of time. This cadence leaves patients without ongoing support, which is especially tough given individuals are likely to encounter stressors upon discharge from treatment that may trigger an urge to use. While many treatment centers assign care managers or sponsors to facilitate the transition back into everyday life, few programs have sufficient bandwidth to accommodate the overwhelming demand.
This is where technology can play an integral role. Technology allows people to carry their support network and programs quite literally in their pocket. It also extends the work of care managers and sponsors, giving them a scalable way to monitor and communicate throughout a patient’s journey.
3. Most people with SUD don’t seek any form of treatment
Astonishingly, only one in ten people with SUD receive treatment of any kind. There are just too many barriers to entry—including stigma, cost and access issues, and a shortage of doctors trained in addiction. Even when treatment is reasonably priced, roughly 40% of people who know they have a substance problem are not ready to stop using—and many feel their usage is not severe enough to warrant treatment.2
Yet this may be technology’s greatest potential to remedy the epidemic: to increase access to and lower the threshold for receiving treatment. Surveys show many substance users maintain a semblance of normalcy—they attend school, hold jobs, and remain in relatively healthy relationships. Providing a digital solution to these individuals enables them to seek help without having to wait for the problem to balloon—and from the comfort of their own daily routines. Though some people will require an in-person intervention, apps can provide an easy onramp, ultimately guiding them to the appropriate intervention.
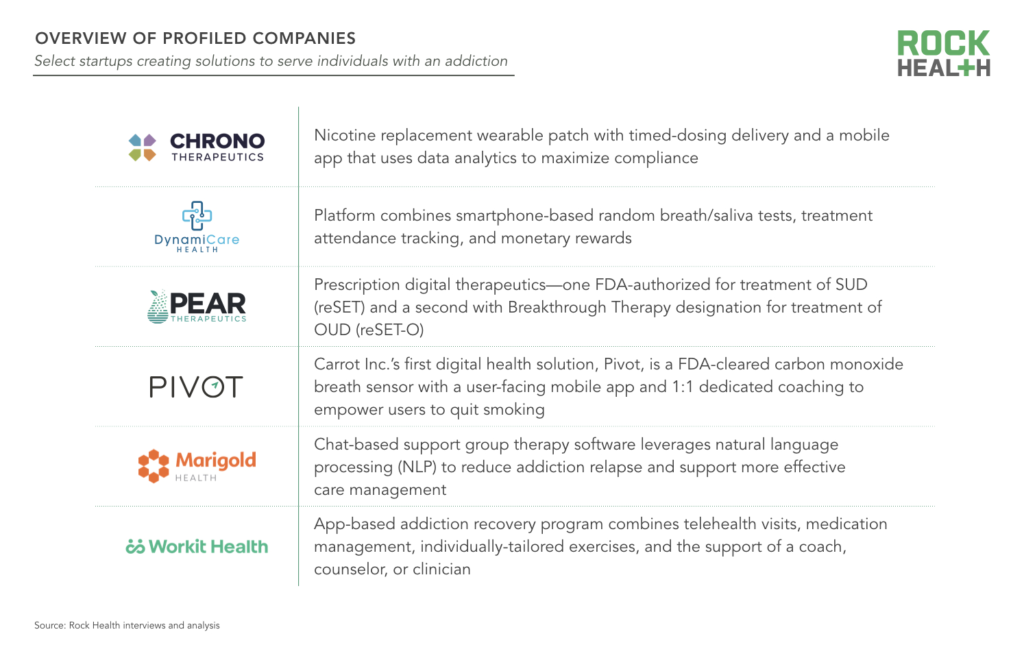
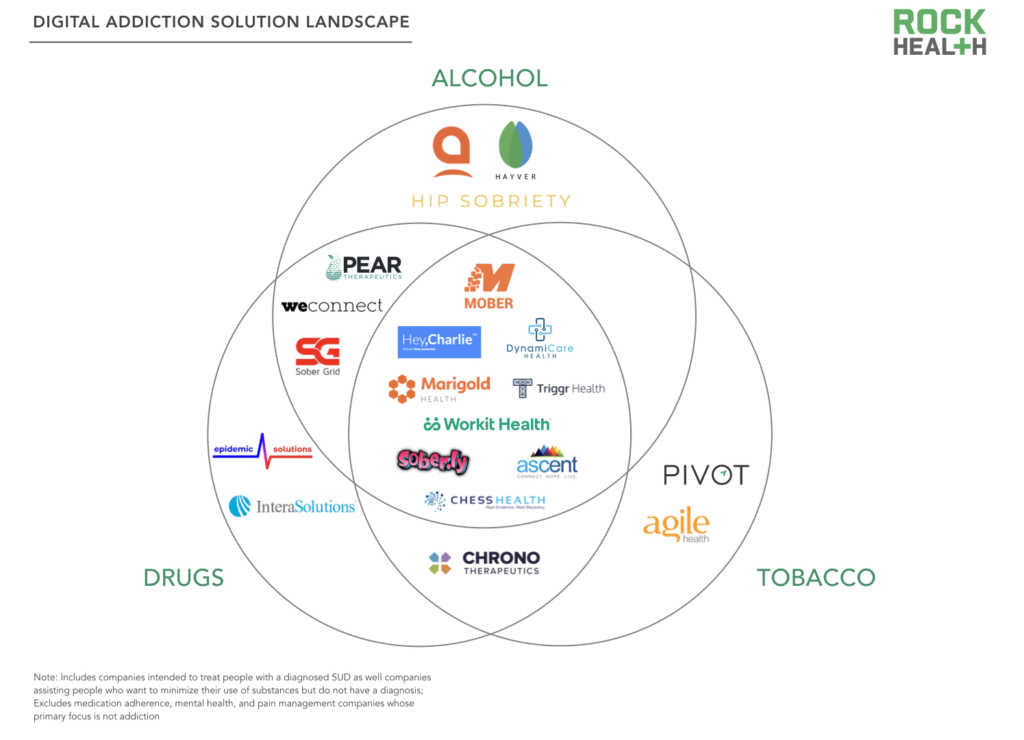
To see what this looks like in practice, we interviewed six startups focused on treating addiction: Carrot Inc. (the creators of Pivot), Chrono Therapeutics*, DynamiCare Health, Pear Therapeutics, Marigold Health*, and Workit Health.
Strategies and business models
Digital solutions for addiction are relatively nascent, with most startups still validating their solutions and broader adoption on the horizon. Though offering a variety of approaches across different substance use disorders, the profiled companies deploy all or a portion of the following four strategies to curb the rate of SUD:
- Pharmacotherapy: pharmaceutical drugs as a treatment to alter neural pathways
- Psychotherapy: psychological methods [e.g. Cognitive Behavioral Therapy (CBT), Acceptance and Commitment Therapy (ACT)] to identify and change troubling thoughts and behaviors
- Contingency Management: tangible rewards (e.g., money) to reinforce positive behaviors, such as attending doctor appointments or completing in-app activities
- Social support: community of other individuals with an addiction to provide accountability and camaraderie through an individual’s quit journey
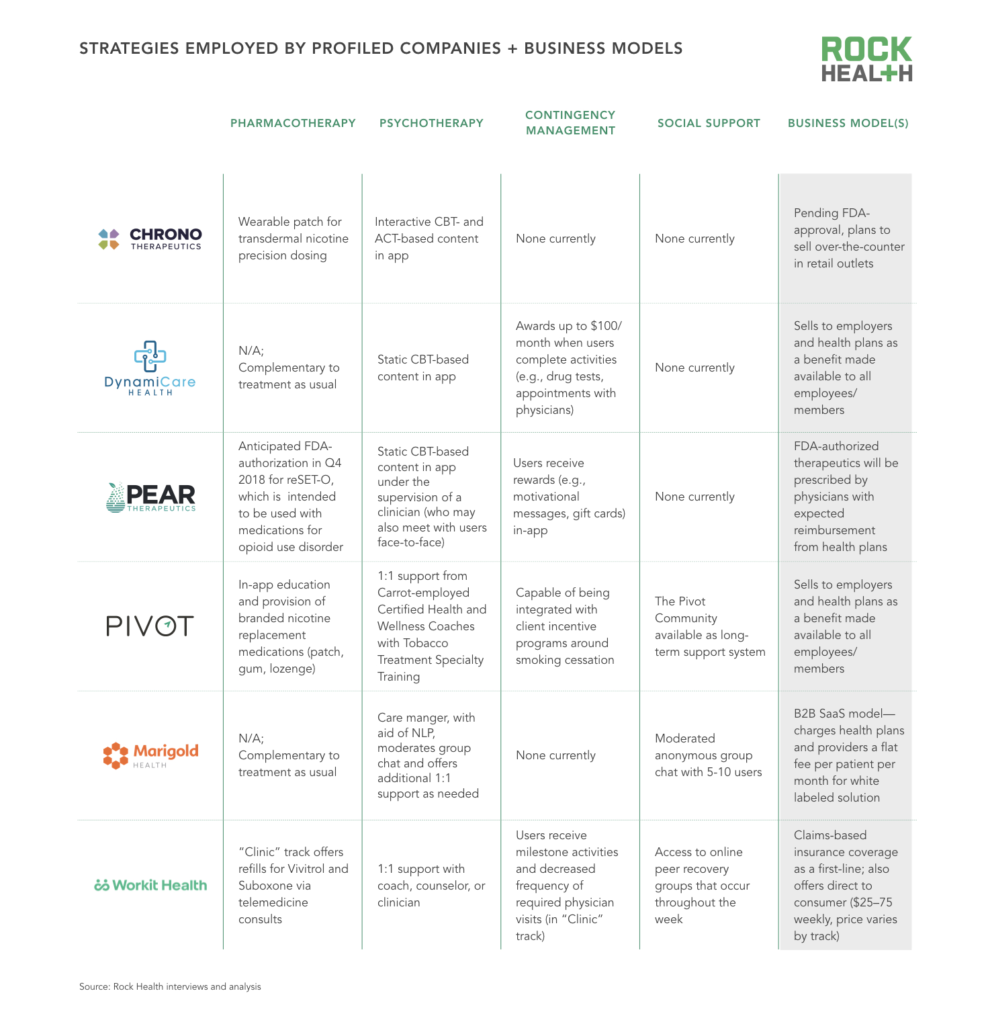
Each profiled company employs a unique combination of the four strategies (based on its target population, business model, and treatment philosophy). Here’s a closer look at how two of these companies, Pear Therapeutics and Marigold Health, think about bringing together the right strategies to create effective, evidence-based solutions.
Pear‘s two digital therapeutics focused on addiction, reSET (for SUD) and reSET-O (for opioid use disorder), combine cognitive behavioral therapy, contingency management, and fluency training3—all under the supervision of a clinician. reSET-O is intended to be used in conjunction with Medication-Assisted Treatment (MAT), and is currently under review by the FDA with Breakthrough Designation. In both offerings, users learn skills to modify their behaviors through in-app modules of static CBT-based content (e.g., avoiding situations that trigger drug usage). After patients complete module activities and test negative for substance use, Pear rewards users with encouraging feedback messages or gift cards.
Pear plans to commercially launch by the end of this year. The aim is for both reSET and reSET-O (following FDA-authorization) to be prescribed by physicians and paid for out of pocket by patients, and ultimately reimbursed by health plans. Pear’s business model thus mimics that of a pharmaceutical drug—and as such, it expects to receive pharmaceutical drug-like reimbursement from payers.
Marigold‘s chat-based group therapy software is a wraparound service to augment a patient’s current treatment regimen. Existing providers—generally care managers at addiction treatment facilities—onboard individuals to the platform upon discharge via a face-to-face consultation. Users join an anonymous support group of five to 10 people with addiction; however, patients are identifiable to a moderating care manager. A natural language processing system flags and deletes abusive messages from patients in real-time, 24/7, and refers concerning messages to the care manager for additional review. Care managers may then reach out to the affected user to offer psychological support and resources.
Marigold licenses and whitelabels its platform to existing treatment providers and payers. In doing so, the company generates patient touchpoints and scales the efforts of existing providers to offer ongoing support to patients and prevent relapse. Certain interactions on Marigold’s platform with a peer support specialist or care management are reimbursable, billed directly by Marigold’s client.
If you’d like to learn more about the strategies and business models of the six profiled companies, email us at partnerships@rockhealth.com.
Areas for continued exploration
We’re excited to see significant progress being made to deliver effective treatment in more accessible ways. But critical questions still remain:
1. With technology front and center, where do humans fit in?
CBT works—what’s up for debate is the degree to which humans need to be involved in delivering it. Relying on technology rather than human staff to deliver content optimizes for scalability. But providers and coaches offer a layer of accountability for users and can draw personalized connections between psychological concepts and individuals. We also look forward to seeing more research on the effectiveness of an online group replicating the social cohesion offered by an in-person group—and if anonymity strengthens or strains the group dynamic.
We’re standing our ground that the human element is critical. People should be augmented by technology—not replaced.
David S. Utley, MD, CEO & President, Carrot Inc.
2. Are current digital offerings doing enough to increase access to care?
Current tech-forward solutions for addiction largely address two of the challenges outlined above—they offer evidence-based care, and do so in a continuous manner. However, the third challenge is tougher to tackle: reaching the roughly 90% of people with addiction who do not currently seek treatment. While many of the platforms aim to increase access to care by lowering the threshold to seek support, most of the solutions require an entry-point via a provider, payer, or employer able to offer these solution. This may still be a barrier to entry for most—particularly the unemployed and uninsured.
Companies that plug into the existing continuum of care miss the biggest opportunity for digital solutions: reaching disenfranchised populations.
Steve Kraus, Partner, Bessemer Venture Partners
3. What are the limitations of digital solutions?
Digital solutions alone cannot remedy the drug epidemic. For individuals with SUD who become gravely disabled and cannot provide for their basic needs of health and safety, digital solutions will not provide enough assistance. Furthermore, SUD often accompanies other serious mental health conditions (e.g., depression, anxiety) and chronic illnesses (e.g., Hepatitis C, HIV/AIDS). As such, some believe digital solutions may be best suited to triage people into care or to provide treatment for less severe populations.
We’re working to build out our snapshot of digital solutions combatting addiction. We’re excited to support entrepreneurs creating solutions so everyone with an addiction can access and afford the care they need, when they need it most. If you are one of those entrepreneurs, let us know about your company!
Further information
For full access to the report—including a case study of each profiled company’s program components and business model—become a Rock Health partner. Email partnerships@rockhealth.com for more information.
Acknowledgements
This report would not have been possible without the help of a number of individuals who have graciously shared their expertise.
Special thanks to Brandon Bergman (Research Recovery Institute), Brian Edquist (Chrono Therapeutics), Eric Gastfriend (DynamiCare Health), Moses Ike (Blue Shield of California), Shrenik Jain (Marigold Health), Steve Kraus (Bessemer Venture Partners), Michael Langer (Pear Therapeutics), Michael Millman (Blue Shield of California), Katherine Monti (Workit Health), Antoun Nabhan (Pear Therapeutics), Andrey Ostrovsky (Concerted Care Group), and David Utley (Carrot Inc.) for their time and insights.
Footnotes
*Rock Health portfolio company
1Reflects age-adjusted rate, calculated using the direct method and adjusted to the 2000 standard population
2Center for Behavioral Health Statistics and Quality. (2016). Results from the 2015 National Survey on Drug Use and Health: Detailed tables. Rockville, MD: Substance Abuse and Mental Health Services Administration.
3Set of question assessments a patient must answer correctly in order to advance in the program

