Seven strategies for telehealth to shape the future of healthcare delivery
Holly May is a consultant at Health Advances.
The standard medical encounter today is local and synchronous: a healthcare provider and a patient must be in the same place at the same time for healthcare delivery to happen.
Telehealth opens a whole new world. It enables remote and asynchronous engagement. The tip of the telehealth iceberg includes the use of videoconferencing to enable a doctor to conduct virtual “house calls” or connect far away loved ones to an important conversation with a physician.
Telehealth holds a lot of promise. But, its potential to improve and streamline healthcare delivery has not been met yet.
Dr. Lee Schwamm is the medical director of telehealth at Massachusetts General Hospital in Boston. In this month’s issue of Health Affairs, he sets forth seven critical strategies for the future delivery of healthcare and outlines the opportunity for telehealth in this brave new world.
1. Understand patients’ and providers’ expectations
- Patients are looking online like never before for health content, but most patients are still concerned about the privacy of their health and medical information. Assurances are necessary that data from telehealth tools and services will be protected.
- Physicians need reliable, high-quality bandwidth to enable these services. New financial models are necessary to ensure physicians can be compensated for telehealth endeavors.
2. Untether telehealth from traditional revenue expectations
- The return on investment for telehealth is long-term, not short-term.
- Providers may not be reimbursed for a remote consultation today, but implementing telehealth has long-term advantages like larger patient panels, more satisfied patients, and the potential to decrease hospitalizations by catching early warning signs between in-office visits.
3. Deconstruct the traditional health care encounter
- The flow of information and materials necessary for a healthcare encounter must be mapped. This is a practice called “value stream mapping” (borrowed from the Lean school of thought). These key steps and processes can be rebuilt in a telehealth environment. For example, virtual visits will require the secure collection of insurance information, health records, and medication lists in advance of an appointment.
4. Be open to discovery
- Telehealth enables more convenient delivery, such as video consultations or cell phone photos of rashes, but it can also create unforeseen, new opportunities.
- For instance, Dr. Schwamm is the director of the Telestroke Network, a hospital-to-hospital network that allows stroke experts at leading academic medical centers to evaluate stroke patients in underserved areas through the use of interactive videoconferencing and the exchange of digital images.
5. Be Bold and Visionary
- “The implementation of telehealth technology is analogous in many ways to that of the automated teller machine (ATM). When it was introduced in the 1970s, the ATM was an expensive, clunky, unfriendly, and inflexible” writes Dr. Schwamm. Back then, ATMs were financial loss leaders; now they are invaluable components of banks. They represent a differentiated service that can drive brand loyalty (think of the latest incarnation: apps from banks that enable secure money transfer or check deposits via photo).
- Telehealth has the potential to improve convenience and patient satisfaction, bring down healthcare spending, and reduce healthcare disparities between urban and rural environments if practitioners dream big.
6. Be mindful of the importance of space
- The physical—and emotional space—matters. Not all residential or commercial spaces have a private, safe place for a virtual visit.
- Patients may not feel as comfortable if the face-to-face interaction is missing, and in turn may withhold personal medical concerns (e.g., birth control or sexual dysfunction).
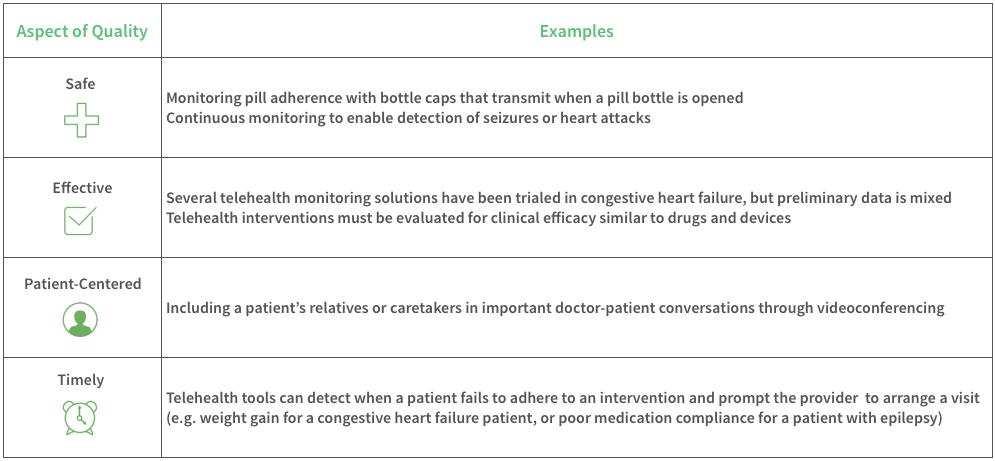
7. Redesign Care to Improve Value
- Lastly, telehealth innovations should increase the quality of care. According to the Institute of Medicine (IOM), quality is defined as: safe, effective, patient-centered, timely, efficient, and equitable.