How to advance healthcare quality though digital health
Successful virtual healthcare services must not merely “design out” the drawbacks of legacy care models. To truly succeed, they must deliver digital innovation that dramatically lowers cost, reduces the load on legacy care providers and infrastructure, and delights patients. But where does healthcare quality show up in the virtual healthcare context, and how should innovators, investors, and healthcare providers approach questions about quality in this paradigm? For a clinician’s point of view, we turned to Simon Mathews, Chief Medical Officer of Rock Health portfolio company Vivante Health, to share a perspective on how digital health can play a role in advancing care quality across four dimensions.
By Dr. Simon C. Mathews, MD
Chief Medical Officer, Vivante Health
Assistant Professor of Medicine and Gastroenterologist, Johns Hopkins Medicine
Not too long ago, quality of care was synonymous with clinical outcomes. In 1999, the Institute of Medicine reported that nearly 100,000 deaths a year were due to medical errors (more recent estimates are closer to 250,000). These statistics changed the narrative on quality, and highlighted that clinical metrics alone do not adequately characterize the overall healthcare experience. As a result, the healthcare community undertook efforts to broaden the definition of quality, advancing a systems-thinking approach that proactively recognizes the complex interrelationships that impact care.
In my role as a gastroenterologist at Johns Hopkins, I’ve seen firsthand this shift to a more holistic approach. During quality improvement meetings, physicians and team members speculate, “How might our next patient come to harm?” Rather than focusing on strengthening clinical metrics, we typically discuss the whole system of care delivery and a patient’s unique challenges interfacing with that system. Fortunately, digital tools can enable this more comprehensive and systems-level view of quality—but what does that actually look like in practice?
A Broader Definition of Quality
Let’s first consider how the current, broadened view of quality can be deconstructed into four principal components—along with how digital health solutions can play a role in improving quality along these dimensions.
- Patient Safety: How do we proactively keep patients from experiencing preventable harm? A classic example here is the use of EHR-based decision support tools to ensure appropriate prophylaxis is selected to prevent blood clots in high risk patients admitted to the hospital. A more recent and not yet widely adopted example is the application of wearables to screen for cardiac arrhythmias, enabling earlier detection of risks that previously were not readily identifiable.
- Clinical Outcomes: Are we providing excellent clinical care? Historically, this question was answered in the form of structural metrics (e.g. 24/7 coverage by advanced endoscopists for emergent procedures), process metrics (e.g. rate of colorectal cancer screenings in ambulatory clinics), and true outcome metrics (e.g. mortality from colorectal cancer). However, as technology capabilities advance, we have the ability to create novel digital outcome measures that offer a more comprehensive and continuous understanding of health and disease.
- Patient Experience: How does the sum of all patient interactions impact a patient’s perception of his or her care? Digital health solutions offer a number of ways to address overlapping facets of experience, including improved in-hospital navigation, online patient support communities and tools, and crowdsourced ratings and reviews. These resources are being driven by the larger trend of healthcare consumerism.
- Value: Are we able to reduce healthcare costs while excelling in the categories above? Decision support tools that assist in selecting the most appropriate diagnostic test for a specific clinical situation, algorithms that use EHR and claims data to identify at-risk patients, and text-based reminders that improve clinic attendance and medication adherence are just a few examples of how technologies can improve patient care and experience while reducing unnecessary costs.
Digital Solutions Can Identify and Bridge the Gap(s)
Traditional healthcare environments are limited by their episodic, in-person interaction with the patient. Digital platforms, in contrast, can connect with an individual in different ways, different places, and at different times. While the marketplace for digital solutions can still benefit from greater validation, the ability for digital health to connect with patients in novel ways should also be recognized as a unique opportunity to improve all four dimensions of healthcare quality.
At Vivante Health, we provide a comprehensive digital solution for self-insured employers and health plans to better manage the digestive health of their populations by improving the quality of care they receive. We combine a digital platform with the personal touch of a care team to deliver a clinically-focused, personalized experience. Our primary approach to optimizing quality and reducing cost is by developing disease and symptom-specific clinical pathways.
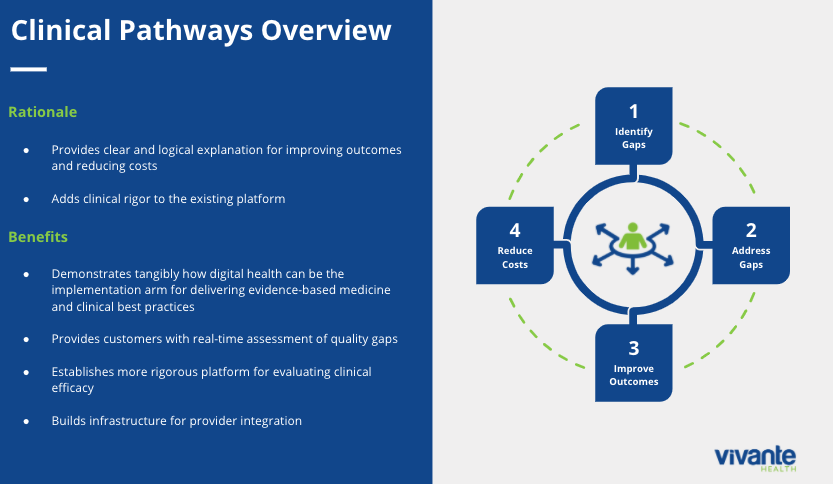
This means recognizing that clinical medicine is complex. One size definitely does not fit all when it comes to digestive diseases, which account for nearly 800 ICD-10 codes. We find that by asking clinically relevant questions that are individually tailored to our members, we can identify the gaps in each person’s care. We then develop and implement a personalized “action plan,” sharing specific tools from our platform to address patient needs. The tools and recommended actions vary by member and may include: dietary counseling with a licensed dietitian, personalized education modules, symptom and food logging, mobile medication reminders, health coaching sessions, and risk summaries that can be shared with their doctors.
We use our digital platform to apply proven, evidence-based interventions in a format that is dynamic and personalized. And importantly, these interventions ensure the Vivante solution is advancing quality for patients and the system across all four dimensions outlined above. Some interventions take the form of surfacing risk factors unknown to the individual that prompt more urgent evaluation (patient safety). In other cases, intervention means regularly measuring validated patient-reported metrics (clinical outcomes) and proactively intercepting a downward trajectory to avoid an unnecessary emergency room visit (value). Vivante also uncovers the larger factors at play, such as healthcare literacy and affordability, caregiver burden, or job-related anxiety and stress which impact an individual’s ability to navigate their illness and the complex healthcare environment (patient experience). In addition, we are incorporating novel biometrics (e.g. microbiome and breath testing) to see if we can augment the personalization we provide. We have been fortunate to realize early promising real-world results, and are looking forward to sharing additional analysis soon.
For physicians, there is an intuitive link between improving outcomes and reducing costs since they see the direct consequences of those who stay on the right path and those who do not. Unfortunately, the latter group experiences more frequent acute care visits, more costly hospitalizations, and greater need for complex drug therapies and interventional procedures. The first step in getting patients on the path to health is understanding on an individual basis which gaps are present. This degree of personalization is truly possible with digital solutions.
Instead of having a limited and rushed annual opportunity to intervene in a traditional clinical setting, digital platforms can act as a near-continuous, virtual safety net, catching those who fall off the appropriate clinical path. More importantly, they provide individuals with innovative tools and interactive support to get back on the right path and regain a positive trajectory. The narrative surrounding digital health is often focused on technology when it should be focused on delivering healthcare quality in all its dimensions. As the capabilities of digital platforms continue to grow, there is reason to be optimistic that healthcare quality will also improve. While technology is an incredible vehicle for digital health, high quality healthcare is the destination.
