AI Is in the Doctor’s Bag—And Primary Care Is Ready to Use It
Thank you to the American Academy of Family Physicians (AAFP) for their support and collaboration, with special gratitude to Shawn Martin; Steven Waldren, MD; Karen Johnson, PhD; Kathy Reid, PhD; and Bethany Burk. Thank you as well to our Primary Care Leadership Committee members: Brent K. Sugimoto, MD, MPH, FAAFP; Jen Peña, MD, FACP, AAHIVS; Ricky Y. Choi, MD, MPH; Jackie Gerhart, MD; Winston Liaw, MD, MPH; Steven Lin, MD; Shweta Maniar; Kameron Matthews, MD, JD, FAAFP; David Rushlow, MD; Nipa Shah, MD; Tina Shah, MD, MPH; and Bill Weeks, MD, PhD, MBA
Primary care is often mentioned as one of healthcare’s top areas for artificial intelligence (AI) transformation. Why? Primary care relies on managing health risks that contribute to a swath of conditions, each with their own complex guidelines—and doing that well has a big influence on health outcomes and cost. Primary care also involves large volumes of patient data and communications, leading to administrative burden and high rates of clinician burnout.
With so much potential for AI to impact primary care, it’s crucial that physician leaders have a seat at the table to shape how AI is developed and adopted in primary care settings. Rock Health and the American Academy of Family Physicians (AAFP) joined forces to explore the potential for AI and digital health to address the challenges faced in primary care, and to strengthen this essential foundation of our healthcare system. Our first step was to directly engage those delivering the care—in an online survey administered between September and November 2024, we asked 1,200+ family physicians and other primary care clinicians about their perceptions and use of digital health and AI tools.1 The majority of survey respondents were family physicians and other primary care physicians, with a small number of non-physician clinicians (NPs/PAs) also represented.
We’ve highlighted some key insights from the survey below to shed light on how family physicians and other primary care clinicians are adapting to AI tools and perceive their impact. For healthcare organizations that deliver primary care or build technologies used in primary care—these insights can help center physician perspectives in strategic decision making.
1. Most respondents are using digital health tools daily, and they’re ready for AI
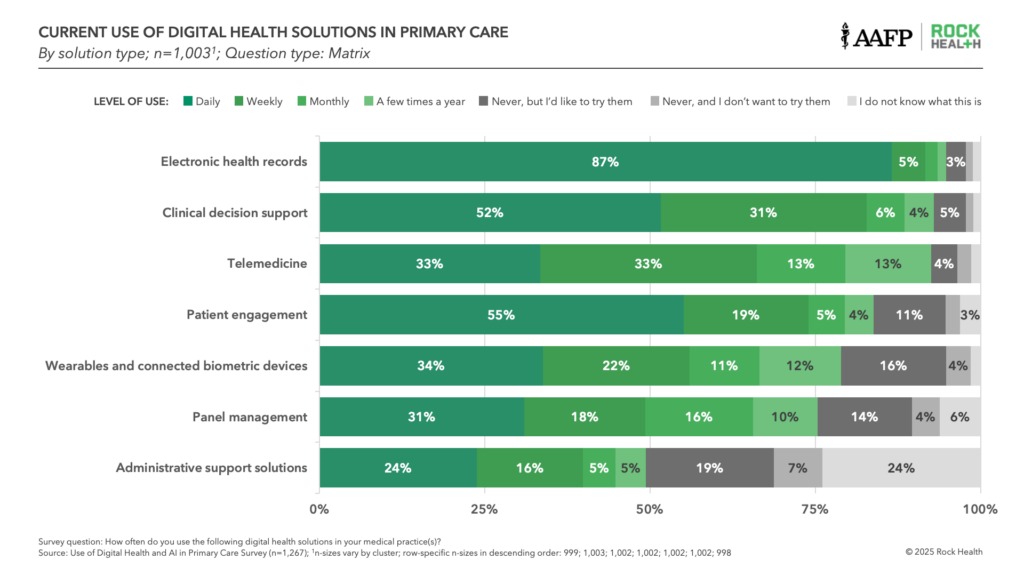
Family physicians and other primary care clinicians reported that they already use digital health tools extensively at work. Not surprisingly, electronic health records were the most prevalent (92% use them at least weekly), followed by clinical decision support (83% at least weekly) and patient engagement tools (74%). One-third reported using telemedicine, wearables or connected biometric devices, and panel management tools in their practice every day. Physicians’ tech savviness extends beyond work—nearly 70% of respondents said they’re likely or very likely to adopt new digital tools personally, and a third said they actively seek out new technologies.
With the rise of AI, family physicians and other primary care clinicians are actively exploring its use both personally and professionally. Sixty-two percent of respondents said they use generative AI tools like ChatGPT outside of work; among those that haven’t, 80% expressed a desire to do so. Eighteen percent said they use AI tools daily in their personal lives—outpacing the general U.S. population, where only 6.4% report daily personal AI use.
Professional use of AI isn’t far behind. Half of respondents reported having used AI tools for at least one use case at work. Thirty-two percent have used AI for clerical support (e.g., message drafting, ambient clinical documentation)—with over half in this category using it daily. Sizable shares have used AI-powered information management (24%) and AI-enabled clinical decision support (23%) tools. More than 90% of survey respondents have tried or are open to trying each one of the professional AI solution categories referenced in the survey, including more nascent AI use cases such as behavioral health support and population health management.

We might have expected that residents and early-career physicians (those within 10 years post-residency) would lead the charge adopting AI tools. However, early-career respondents were no more likely to have tried AI solutions than their more established colleagues.
2. Respondents have limited involvement in AI tool selection, purchasing, and development
Despite being on the front lines of care, most family physicians and other primary care clinicians reported having limited influence over the AI tools available in their practices. Sixty-five percent said they have limited or no input on AI purchasing decisions.
This gap isn’t entirely surprising considering how the practice landscape has shifted from physician-owned and -led practices toward more of an employment model. AI solution purchasing often happens at the organizational level, driven by health system executives or other leaders outside of the practice setting. Given the high costs, inherent risks, and desire for consistency across organizations, top-down decision making is the norm. However this also creates vulnerability: AI’s long-term success in primary care will ultimately depend on the buy-in of those using the tools.
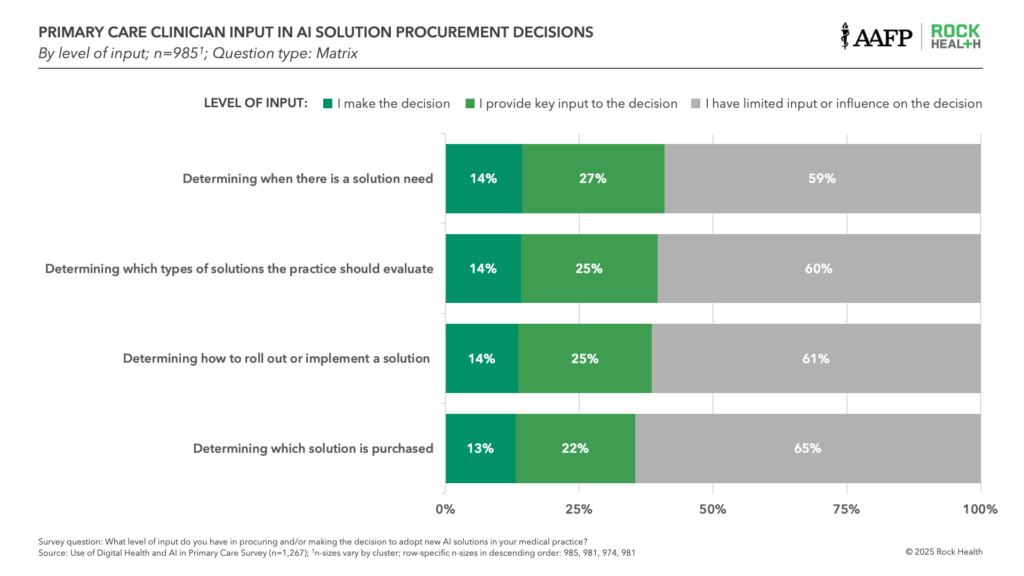
User buy-in can make or break the trajectory of newly launched technologies. When physicians don’t see their input being valued at their organizations, the effects can be long-lasting. For instance, many providers felt left out of EHR selection and optimization in years prior—and in our survey, 55% said EHR charting and documentation was their top operational challenge, rising to 62% among those reporting burnout.
3. Survey respondents expect specific gains from AI—but have significant concerns
Primary care physicians have mixed feelings about AI’s impact over the next three years—optimistic about some aspects but skeptical about others. Many said they believe AI will improve their own clinical efficiency, including improving time to diagnosis (73% expect positive impacts), diagnostic accuracy (66%), and appropriateness of treatment plans (66%). Most expect it will improve their wellbeing (70%) and workload (66%).
But, despite these expected benefits, respondents were skeptical that patients would experience the same upside. About half of respondents said they don’t expect gains from AI to positively impact patient satisfaction (47%), the personalization of care (52%), or clinician-patient relationships (55%) over the next three years.
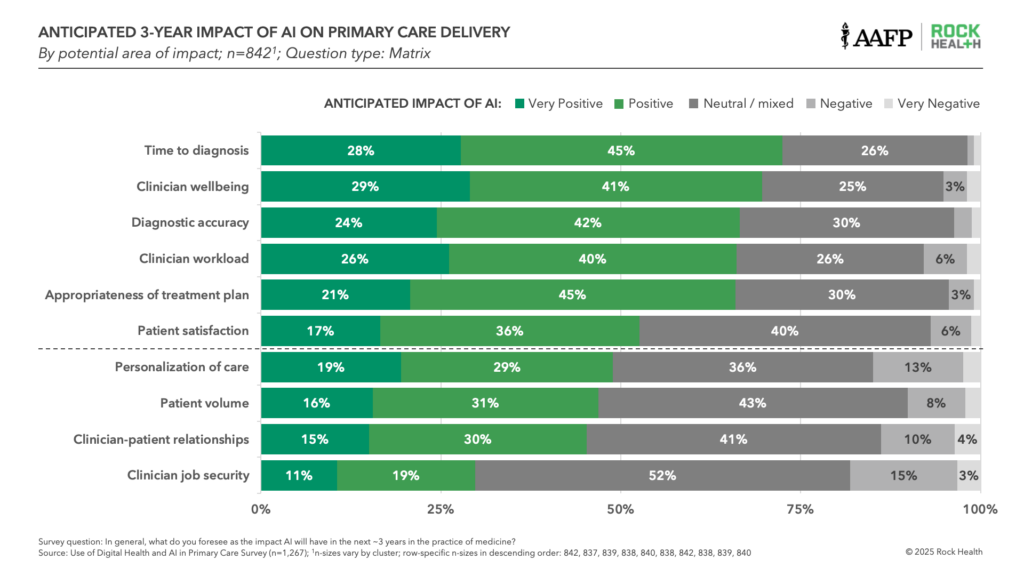
Family physicians also hold concerns about AI in the workplace. Eighteen percent fear that AI will have negative or very negative impacts on their job security, while another 52% are still unsure. Eighty-one percent want more training to fully trust AI solutions at work, signalling hesitancy to adopt these tools into their workflows. Nearly 70% also want medico-legal protections before they trust AI tools and 64% want education on legal, liability, and malpractice risks—likely reflecting concerns about increased liability. Finally, 68% are looking for ethical guidelines on how to best use AI in their practice.
Engaging primary care physicians beyond the early stages of adoption
The survey data confirms that family physicians and other primary care clinicians have already begun using AI solutions—and they’re eager to explore and expand utilization beyond early use cases. With 39% of respondents in our survey reporting burnout, most seem willing to try new tools that could offer relief as a starting point.
That said, trying is different than fully trusting, and most want additional training and legal protections before embracing AI. Since most physicians and other clinicians aren’t involved in AI purchasing and rollout, sustaining adoption will require concerted efforts to actively engage the clinical workforce. If this gap between clinician end-users and AI buyers continues, it could present significant challenges—particularly as the pace of transformation accelerates.
For AI to transform primary care, practicing physicians need to be engaged early and often. That’s a goal of our collaboration with AAFP, which explores how to make meaningful AI-enabled changes in primary care and how to best foster responsible development and deployment. We will use these survey results, plus insights from a multi-stakeholder convening on how AI and digital health can strengthen primary care, to publish a joint paper in June 2025. The paper will provide actionable insights for key stakeholders (e.g., health systems, tech companies, and AI startups) to deliver solutions of maximum value to primary care as they drive AI forward.
Tap into insights and strategic guidance for enterprise companies with Rock Health Advisory.
Join us in building a more equitable future at RockHealth.org.
Stay plugged into the Rock Health community and all things digital health with the Rock Weekly.
About AAFP
Founded in 1947, the AAFP represents 130,000 physicians and medical students nationwide. It is the largest medical society devoted solely to primary care. Family physicians conduct approximately one in five office visits — that’s 192 million visits annually or 48 percent more than the next most visited medical specialty. Today, family physicians provide more care for America’s underserved and rural populations than any other medical specialty. Family medicine’s cornerstone is an ongoing, personal patient-physician relationship focused on integrated care. To learn more about the specialty of family medicine and the AAFP’s positions on issues and clinical care, visit www.aafp.org. For information about health care, health conditions and wellness, please visit the AAFP’s consumer website, www.familydoctor.org.
Footnotes
- The survey was administered to 1,267 respondents between September 18 and November 4, 2024 via web-based survey platform


