Why consumers want their health records
Efforts to get patients involved in their personal health records (PHRs) have become a persistent challenge for the Health IT world. In the face of many unsuccessful initiatives (e.g., Google Health ), we sought to understand whether patients actually want their records, and if working towards overcoming these challenges is worth the effort. As another follow up post on our Digital Health Consumer Adoption survey, we examined the current state of patient engagement and adoption of PHRs to evaluate the successes of these initiatives thus far as well as future opportunities for improvement. We covered overall rates of adoption, reasons for interest in downloading, and breakdowns across demographic groups.
In our landmark report, we found that 24% of respondents (n = 4,017) had either asked for or downloaded their personal health records. In addition, 63% of those who had not yet done so (n = 3,040) were interested in obtaining their records. Clearly, there is interest from consumers across all demographics. By empowering consumers with their personal health records, they can become more involved in their health and make informed decisions.
Having access to your health information allows you to be a full participant in your care. If you are more knowledgeable about your health, you have a much higher likelihood of having a thoughtful, complete, and worthwhile conversation with your doctor.
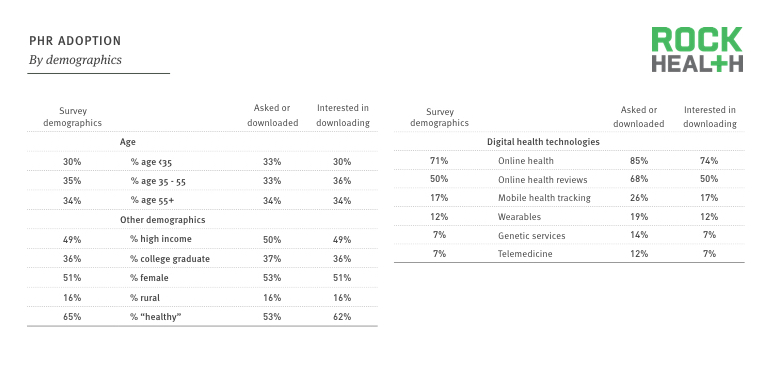
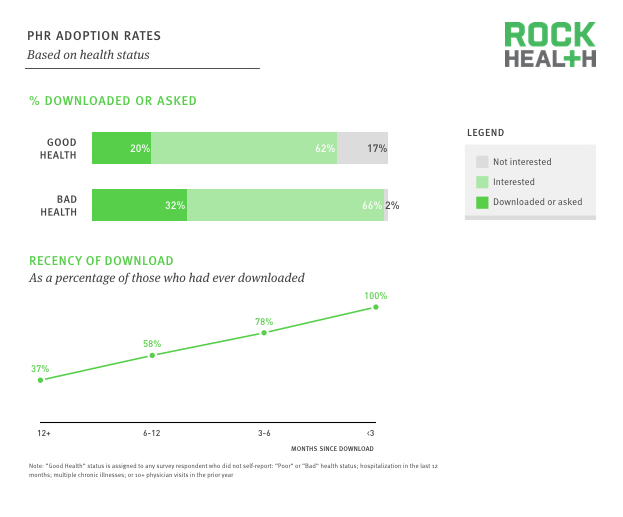
Similar to our findings throughout the Digital Health Consumer Survey, there were no significant differences across the demographics of age, gender, income, education, and geography between those who had asked for or downloaded their PHR and the general population. However, adoption of other digital health technologies was an indicator of health record adoption. Among those who had downloaded their health records, rates of adoption across the six core digital health categories (online health information, online health reviews, mobile health tracking, wearables, genetic services, and telemedicine) were significantly higher. Overall adoption rates were also higher among those who had downloaded their health records. The percentage of super adopters (individuals who had adopted five or six technologies) was 7% among those who had downloaded their records, versus 2% in the general population. Among the respondents who had asked for or downloaded their data, 42% had done so within the last 6 months, and 21% had done so within the last 6-12 months.
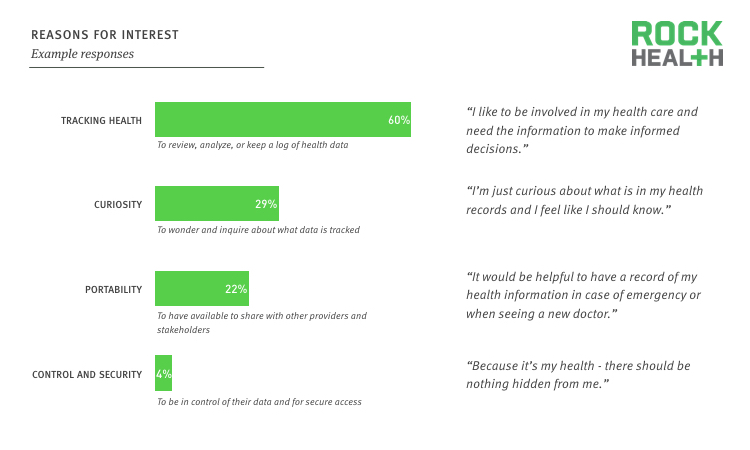
For those who were interested in obtaining their records, we asked why they were interested in doing so. These free responses were broken into four categories: tracking health (60%), curiosity (29%), portability (22%), and control and security (4%).
The average amount that consumers were willing to pay to obtain their electronic health records across all categories was $12.69. This number was fairly consistent across the categories of tracking health, curiosity, and portability. However, of those who were interested in obtaining their records for control and security, this number skyrocketed to $21.16.
Looking across demographics, females were more interested in downloading their health records for tracking health, portability, and curiosity. In addition, those between the ages of 35 and 55 were most interested in tracking their health. Those who were interested in obtaining their health records for portability reasons were more likely to have at least a college education.
Adoption status across the six core metrics was not found to be a significant indicator of interest in downloading records of those who had not already done so. General adoption status was also not a significant factor. However, health status and consumerism were significant for those who were interested. Consumer index was used as the consumerism metric, which was based upon a scoring of questions surrounding responsibility for one’s own health, active management of one’s own health, and willingness to pay out-of-pocket for healthcare expenses. Health status was dependent on self reporting of health, hospitalization in the last 12 months, presence of multiple chronic illnesses, or more than 10 physician visits. High consumer index individuals were more likely to have interest, and consumers with bad health were also more likely to have interest in obtaining their electronic health records.
While there is a high ceiling for future adoption of PHRs, there are significant challenges that need to be overcome in order to convert this interest into active use. One significant problem is how difficult it is to obtain past records as well as records across providers. In 2004, only 21% of doctor’s offices used electronic records. While this number has grown to 83% in 2014, most of those records have not been consolidated, and there are logistical challenges such as privacy concerns and faxing of documents that make it difficult and time consuming to do so. Finally, many people simply don’t know what personal health records are, or what downloading means. One respondent said he wanted his records “Because I can keep it hidden,” showing a misunderstanding that the original records are not altered by downloading them.
There are numerous potential benefits associated with patients downloading their personal health records. Giving patients the ability to access and share their personal health records allows for better coordination between providers, which can cut down on duplicative procedures and improve the data available for successful diagnoses. There are also potential annual savings of up to $79B associated with reduced cost and waste, as well as significant reduction of medical errors. Moreover, enabling patients to download their health records provides a way to double check for accuracy, remember details that may have been forgotten, and discover ways to improve and track their health. In order to capitalize on this interest, however, a lot more work must be done.
Over the last few years, the US government has enacted several measures to tackle some of these issues. In 2009, with the establishment of The American Recovery and Reinvestment Act, doctor’s offices and hospitals were given incentive payments to begin the first step of adopting EHRs. In 2010, HHS implemented Blue Button, a simple way for downloading online health information, in order to facilitate data transmission to patients. However, vast improvements are needed to make these tools successful. For instance, simplifying portals and reducing the steps required to access and download a patient’s health records should increase adoption. Encouragement from providers may be another key intervention to convince people to act.
With the individual in control of his/her own health records, this could greatly improve interoperability between and across providers to help patients receive the best, most holistic care available.