Brushing up on oral health: The case for expanded oral health innovation and investment
Acknowledgments: Thank you to CareQuest Innovation Partners for their support and collaboration on this work. We would like to give special recognition to Katie D’Amico, Vice President of Growth & Innovation for her contribution, as well as acknowledgments to Kate Lewis, Julia Green, Jeremy Jonckheere, Michael Pimental, Adam Schulhof, Mackenzie Richter, and Amir Reuveny.
Oral health is about more than just clean teeth; it’s a key component of overall health. While most people are familiar with dental care such as teeth cleanings and cavity fillings, fewer know that there is a relationship between oral health—i.e. the health of one’s teeth, gums, tongue, jaw, and surrounding structures—and general health. Oral health plays a significant role in systemic health issues like sleep disorders, diabetes, Alzheimer’s, and heart disease, and the connection between oral and general health is heightened at transitional life stages like pregnancy.
It makes sense that many overlook the interconnectedness between oral and general health, because oral health is most often treated and insured separately from general healthcare. However, fragmented medical and dental care contributes to increased health system costs and poorer patient outcomes; higher rates of emergency department utilization, opioid use for unmanaged dental pain, and adverse pregnancy outcomes are just a few of these impacts.
There are signs of change. Early market leaders are integrating oral and medical health services, and new technologies are improving patient workflows and care coordination—together reducing cost and improving clinical outcomes. Rising investment activity is also a promising signal, with capital raises at oral health startups like Overjet ($53M raised in March 2024), Pearl ($58M in July 2024), and Perceptive ($30M in July 2024) making headlines in recent months. This article is designed to help healthcare leaders “open wide” to the current market forces, startup ecosystem, innovation potential, and action steps needed to work toward whole-person care.
“Thinking about dental care makes sense for a health system to say, ‘I really want to get my arms around [patients’] whole health. How do I do that?’ Well, it turns out dentistry is much more relevant than we thought. That’s what the data is showing. That’s what the dentists have been telling us for a long time. You’re starting to see a recognition of that, and then you’re starting to see business decisions to drive that and really bring that to life.”
—Dr. David Kim, CEO, MemorialCare Medical Foundation
Market dynamics: Forces shifting the oral health landscape
Oral health and general medicine evolved as separate clinical practices in the United States, ingraining systemic barriers between the two that impact patient access, care coordination, interoperability, and innovation. These barriers manifest in the ecosystem as the following constraints:
- Medical and dental silos: Legacy practices have contributed to siloed medical and dental care systems. Dental providers are limited by scope of practice restrictions to what general health needs they can address, even if these needs have oral health connections (and vice versa). For example, despite the strong link between human papillomavirus (HPV) and oral/oropharyngeal cancers, dentists in most states aren’t allowed to administer HPV vaccines to their patients. Separate dental and medical insurance plans, as well as fragmented diagnostic codes and reimbursement processes, reduce incentives for providers to deliver coordinated care even if they are licensed to do so. Disconnected patient records and workflows make it difficult to coordinate treatments or refer patients. For example, in one study only 4% of patients reported ever being referred to a primary care provider by their dentist.
- Low awareness of oral health’s importance: Oral health is often deprioritized or omitted from medical school curricula and patient education, resulting in many medical providers feeling underprepared to identify oral health issues or make necessary referrals. In addition, consumers are often unaware of the close relationship between oral and systemic health. In any given year, 108 million Americans visit a medical provider but do not see a dentist, including more than 60% of children ages one through four.
- Cost and access barriers: Access to and affordability of health services can vary between oral and medical care. Sometimes, these barriers stem from the fact that oral and medical care are covered under separate health plans; other times they relate to the fact that many people are under- or uninsured when it comes to oral health needs. Sixty-nine million U.S. adults currently live without dental insurance coverage, including 25 million on traditional Medicare plans, for whom basic dental services like routine cleanings, fillings, and tooth extractions aren’t covered. Dental coverage is mandatory for children in Medicaid and CHIP programs, and typically includes routine care like exams and cleanings. Yet, for adults coverage varies widely, with only some states providing dental benefits as part of Medicaid.
Fragmented coverage and out-of-pocket costs exacerbate other systemic barriers to healthcare like provider availability, transportation issues, and long wait times for appointments. This compounds racial, ethnic, and social inequities in oral health. For example, a 2023 report from the Kaiser Family Foundation found that Hispanic (45%) and American Indian/Alaska Native (45%) adults were significantly more likely than white adults (34%) to report going without a dental visit in the prior year.
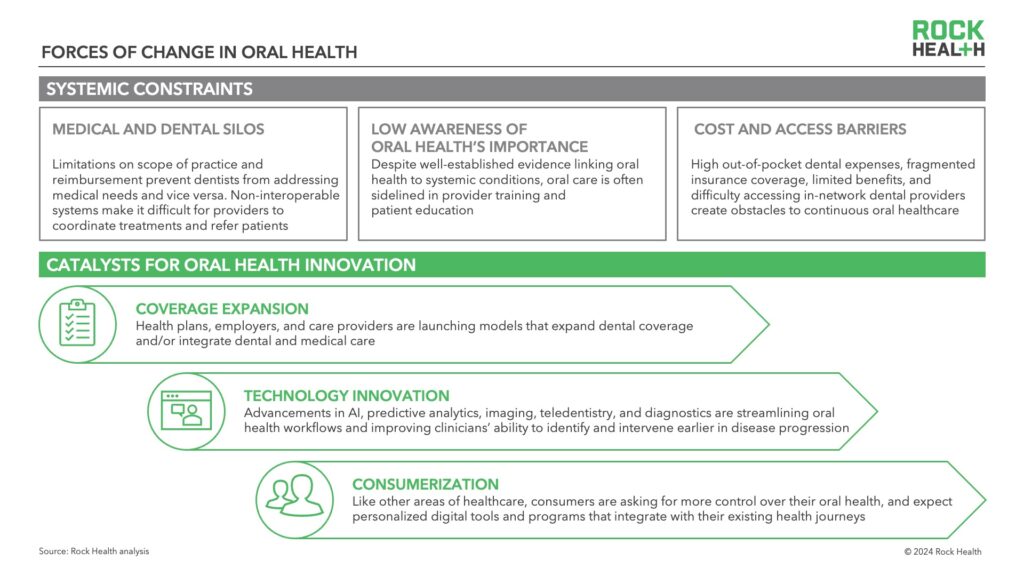
Yet, the following market forces are challenging the separated status quo and catalyzing oral health as an innovation area:
- Coverage expansion: Payers, employers, and Medicare and Medicaid programs are launching new plan designs and care models that expand oral health coverage and/or integrate oral and general health. Medicare Advantage (MA) plans have been early movers here; as of 2023, 97% of individual MA plans offer a dental benefit. Additionally, six states have expanded adult dental benefits for Medicaid members so far in 2024. Alternative payment models like value-based care arrangements are also beginning to emerge in dental and incentivize preventative care.
- Technology innovation: Tech advancements including AI, predictive analytics, teledentistry, and precision imaging are helping providers identify and treat oral conditions earlier and coordinate care across oral and medical domains. According to a 2021 CareQuest Institute survey, 96% of oral health providers believe data-driven decision support technologies improve patient care, signaling high real-world acceptance. New tech also strengthens the provider-patient relationship by involving patients more in their treatment decisions. Real-time imaging, for example, helps patients see and understand their conditions, making them more likely to agree to and follow through with treatment plans.
- Consumerization: Like other areas of healthcare, consumers are asking for more control over their oral health with access to information, tools, and personalized care options. With consumers already using wearables, connected devices, and telemedicine for healthcare needs, there’s a growing expectation for more flexible and accessible oral health solutions that integrate with consumers’ existing healthcare data and devices.
Digital health startups are building on these market forces to launch solutions that improve oral and overall health efficiency, experience, and outcomes; below, we outline these innovation categories. We also see innovation evolving not just to optimize oral care, but also to build bridges needed between oral and medical care—something we talk about later on.
Digital solution archetypes supporting oral health innovation
Historically, digital health startup activity in oral health is limited compared to other medical specialties. Contributing factors include siloed oral and general healthcare, as well as popular misconceptions about the size of the oral health market and its impact. The current oral health startup landscape is concentrated on dental health startups, specifically preventative, diagnostic, and restorative dental services. On average, funding for U.S.-based digital dental health startups accounts for less than 2% of overall digital health funding annually, according to Rock Health’s Digital Health Venture Funding Database.1 However, we’re at an inflection point: 25% of all deals and 20% of all investment dollars for digital dental health startups occurred between 2023 and H1 2024, suggesting investment momentum in the category.2
To assess the current innovation landscape, we aggregated and analyzed digital dental health startup, funding, and partnership activity to identify top digital solution archetypes attracting market attention.3
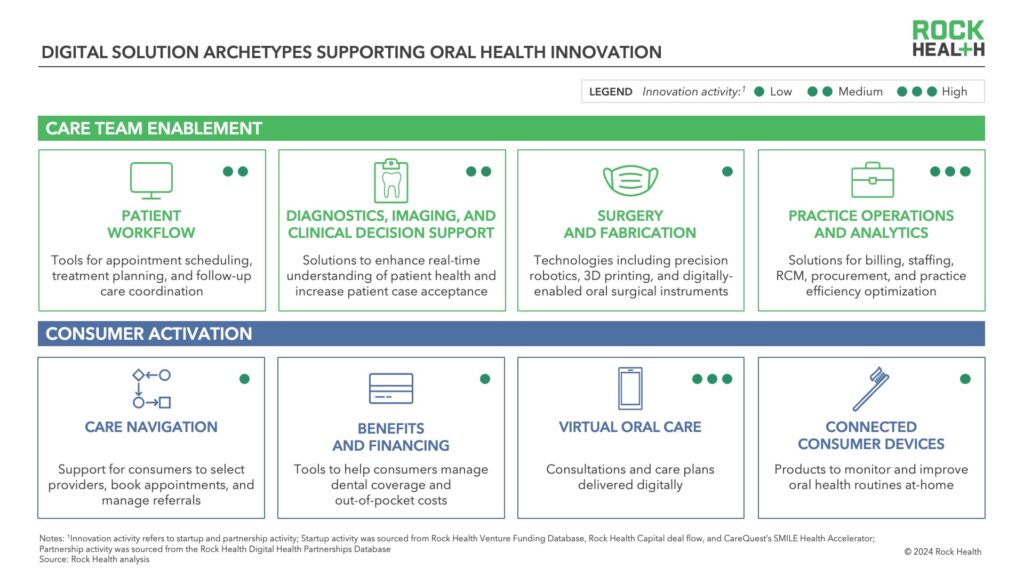
These archetypes fall under two main service categories: care team enablement and consumer activation.
Care team enablement: Digital tools that help oral health providers deliver patient care efficiently and effectively by simplifying workflows, improving communication between team members, and offering data-driven insights to improve care planning. These tools also help streamline care across providers (e.g., coordinated referrals) and alternative sites of care.
- Patient workflow: Software that coordinates the patient journey from appointment booking to follow-up and referral management, improving administrative efficiency and enabling seamless handoffs between care providers.
Example digital health companies: Peerlogic, Heygent AI, PracticeMojo, mConsent - Diagnostics, imaging, and clinical decision support: Technologies such as x-rays and intraoral cameras, often integrated with AI-enabled clinical decision support systems, allow clinicians to assess patients’ oral health in real time, show areas of concern directly to patients, and streamline treatment planning.
Example digital health companies: VideaHealth, Synbase, Dexis - Surgical and fabrication: This category includes advanced technologies such as precision robotics for surgery, 3D printers for dental implants and appliances, and digital tools for oral surgeries and procedures. While innovation activity is still relatively low in this category, new solutions show promise in reducing costs and improving procedural accuracy, particularly for complex procedures and personalized oral devices.
Example digital health companies: Perceptive, Roland DGA, Planmeca - Practice operations and analytics: These tools optimize practice management, including billing, staffing, and supply procurement. Growing startup activity in this category reflects trends in digital health funding for nonclinical workflow solutions, bolstered by AI-based process innovation.
Example digital health companies: Zuub, CareStack, CureMint, tab32
Consumer activation: Digital tools that engage, educate, or otherwise empower patients to take active roles in their oral health. These tools use virtual platforms to offer easy access to oral health information, encourage self-care and regimen adherence, and keep communication open with providers, leading to better health and a more positive patient experience.
- Care navigation: These platforms help consumers find oral health providers, book appointments, and manage referrals. Many also integrate with provider-facing patient workflow tools, enabling seamless care management between provider and patient.
Example digital health companies: Smylen, Opencare, Zocdoc - Benefits and financing: Tools in this category help consumers manage their dental coverage, employment-based benefits, and out-of-pocket costs. As integrated medical-dental insurance models continue to evolve, this category may see increased activity.
Example digital health companies: Flossy, PatientFi, Bento - Virtual oral care: Telehealth platforms facilitate digital oral consultations, most often for patient intake, follow-up visits, or emergency dental consultations. High startup activity in this category mirrors overall sector trends, when tailwinds from the COVID-19 pandemic driving startup launches and funding to virtual care.
Example digital health companies: Dentistry.One, ToothLens, Grin, Dentulu - Connected consumer devices: At-home smart devices like connected toothbrushes and oral sensors fall under this category. As these devices become more advanced, they’re more likely to offer real-time feedback and personalized recommendations that are of higher value to consumers.
Example digital health companies:4 quip, Feno, BLÜ
As the oral health market evolves, we expect that these archetypes will expand to reflect a broader digital solution ecosystem, encompassing more nascent categories like oral microbiome health and integrating deeper with general health needs. Dental startups raising capital today are well positioned to lead this broadening, and companies operating in adjacent areas like chronic disease management, general virtual care, and remote patient monitoring could find opportunities to broaden their offerings into oral health as demand grows.
Opportunity areas for oral health innovation
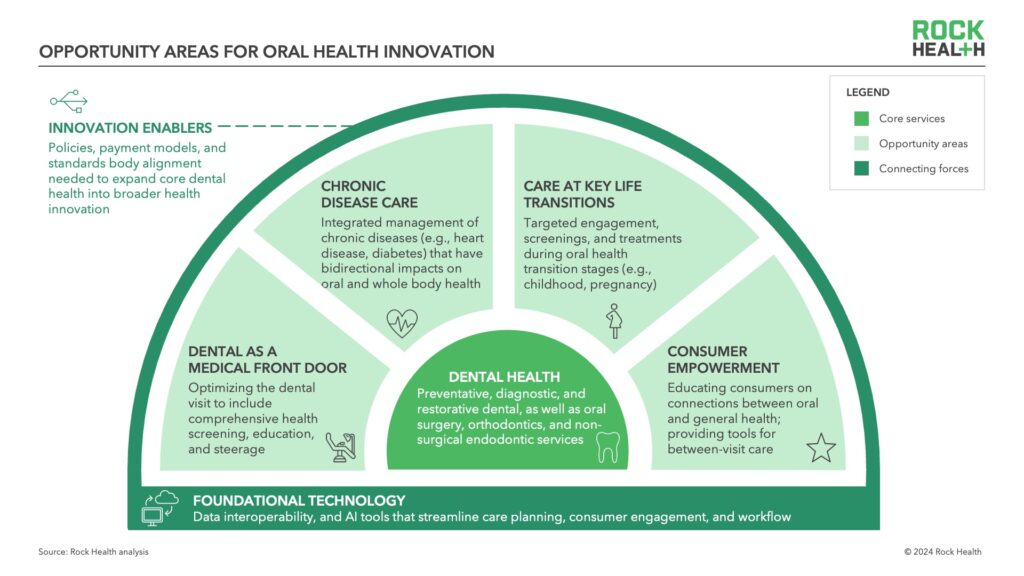
Oral health innovation isn’t just about launching new tech—it also means furthering care models that connect oral health to whole-person care. We’ve outlined four key opportunity areas beyond core dental health where innovators can introduce new programs that push forward oral health innovation, bridge the gap between services for a more integrated patient journey, and offer strong ROI and potential market share growth.
- Dental as a medical front door: Dental appointments, which are recommended twice a year, can act as a gateway to other healthcare services. Each year, 27 million Americans visit the dentist but not a physician, presenting an important opportunity to integrate basic health screenings into routine dental care and reach patient populations without regular medical care visits. Many dentists are already engaging with patients about their general health at the start of a new patient visit: 90% ask patients about their health histories and medications, and 57% of dentists collect at least one vital sign for every patient at every visit.
By enhancing dental appointments to screen for wellness needs, early indicators of disease, or social determinants of health barriers, oral health providers can encourage behavior change and provide actionable next steps. For example, if dental visits screened for prediabetes—a condition affecting over 98 million Americans, 90% of whom are unaware they have it—early detection could prevent disease progression, saving an average of over $2,500 per prediabetic person per year. Startups are already working to expand what’s possible in the dentist’s chair, like OralDNA, which offers “chairside” salivary diagnostics kits. - Chronic disease care: Chronic conditions like diabetes, heart disease, and Alzheimer’s have bi-directional relationships with oral health. Poor oral health exacerbates these conditions through chronic inflammation and bacteria entering the bloodstream. People with diabetes are up to three times more likely to develop periodontal disease; treating periodontal disease in this population can save individuals with diabetes nearly $6,000 in healthcare costs per year. Coordinated care models can use dental visits to help monitor patients’ chronic conditions and build healthy habits for disease management. Payers can also engage members with or at-risk for chronic diseases with targeted oral care engagement and appointment reminders. Aetna, using an integrated medical-dental coverage model, saved nearly $5,700 per engaged member over three years due to proactive outreach about oral care appointments to at-risk covered members.
- Care at key life transitions: Life stages like pregnancy, early childhood, and aging are important moments when oral and overall health are even more closely linked. For instance, gum disease during pregnancy can contribute to preterm birth risks, yet less than half of pregnant women see a dentist. In early childhood, delayed dental visits lead to higher costs per young person, decreased academic performance, and more procedures to treat early childhood caries (tooth decay). A study of over 40,000 children found that delaying the first dental visit until age four resulted in an average of 3.6 additional procedures per child. There’s an opportunity for payers, providers, and startups to deliver targeted touchpoints, like guidance on preventive oral care for children or reminders for prenatal dental checkups, to significantly reduce downstream healthcare costs and improve outcomes.
- Consumer empowerment: As consumers increasingly view oral health as part of their overall wellness journey, there’s a growing demand for personalized, holistic oral care solutions. Younger generations in particular see oral health as connected to their mental health and overall wellbeing. In-home devices, such as connected toothbrushes, can provide consumers with real-time feedback and offer action steps for improved self-care. Virtual coaching and personalized care plans can engage consumers between dental visits, helping them establish healthier habits. There’s also an opportunity to integrate oral health assessments and treatments into other aspects of health, such as mental health, sleep health, and chronic disease prevention. By connecting oral health with lifestyle coaching, nutritional counseling, and disease risk screenings, innovators can position oral health as a cornerstone of consumer health goals and routines.
“Most consumers don’t think of oral health as a wellness investment. There’s an opportunity to help consumers understand that taking care of your oral health is like eating right and exercising, in terms of reducing inflammation and disease risk.”
— Brant Herman, CEO and Founder, MouthWatch and Dentistry.One
Connecting forces
Meeting these opportunity areas isn’t easy: it requires practical changes across technology, practice, and policy. Founders, investors, and healthcare leaders can drive forward some of the required shifts, like promoting integrated solutions. Interoperable electronic medical records (EMRs) and electronic dental records (EDRs) are also essential, as providers face consistent barriers to submitting referrals, identifying a patient’s medications, and requesting medical history. Systems like Epic’s Wisdom module and Dentrix Connected’s APIs, are starting to bridge these gaps, enabling providers to gain a full picture of a patient’s health and identify health risks earlier, such as the connection between gum disease and heart disease. Policy support will also be important in this domain, integrating oral health within national interoperability efforts.
Larger systemic changes—specifically medical and dental curricula changes, payment model evolutions, and scope of practice expansion—will require coordinated efforts from key stakeholders like policymakers, professional organizations, standards bodies, payers, and providers. Expanding Medicare and Medicaid to include routine dental services is an essential and widely-supported change, with 92% of U.S. voters supporting the addition of a dental benefit to Medicare according to one national survey. Integrated payment models that track outcomes across both medical and dental domains are also needed to pave the way for value-based care in commercial plans. Policy and regulation reform is needed to incentivize dental teams to perform certain medical tasks like administering vaccines, and enabling medical providers to address basic oral health needs can reduce reliance on emergency visits and other avoidable high-acuity care. In addition, harmonizing standards between medical and dental bodies will ensure consistent care protocols, especially for specific conditions or life stages like pregnancy.
“Innovating in oral health requires breaking down barriers—in scope of practice, reimbursement, and infrastructure, including access to products and electronic health record interoperability—all while fostering a culture of collaboration and mutual respect between medical and dental providers.”
— David Kochman, Vice President, Chief Corporate Affairs Officer, Henry Schein
The path forward for oral health innovation
The opportunity to expand oral health’s role in healthcare is clear. By exploring new digital solutions, investing in connecting forces, and pursuing strategic opportunities, healthcare leaders can unlock the full potential of more integrated health, inclusive of oral health. Driving critical transformation will require participation from payers, policymakers, patients, and providers—it’s time to sink our teeth in.
To tap into insights and strategic guidance—or work with us to advance thought leadership in the ecosystem—reach out to advisory@rockhealth.com.
Join us in building a more equitable future at RockHealth.org.
And last but not least, stay plugged into the Rock Health community and all things digital health with the Rock Weekly.
Footnotes
- Funding for U.S.-based digital health startups addressing dental health and raising $2M+ comprised, on average, 1.2% of overall U.S. digital health funding each year from 2011-H1 2024.
- This analysis accounts for all venture deals and funding dollars transacted since 2011. For the overall digital health market, these figures were 15% and 14%, respectively.
- Startup activity was sourced from Rock Health Venture Funding Database, Rock Health Capital deal flow, and CareQuest’s SMILE Health Accelerator. Partnership activity was sourced from the Rock Health Health Digital Health Partnerships Database.
- Top makers of connected oral care devices include enterprises and CPG companies (e.g., Colgate-Palmolive, Procter & Gamble, Phillips); however, examples in the piece focus on digital health companies.

