Consumer adoption of telemedicine in 2021
Thank you to the Stanford Center of Digital Health for their continued collaboration on this work, with special gratitude to Natasha Din, MD, Clark Seninger, MBA, Sravya Rallapalli, Ashish Sarraju, MD, James Tooley, MD, Krishna Pundi, MD, Mario Funes-Hernandez, MD, and Mintu Turakhia, MD.
Nearly two years into the COVID-19 pandemic, more consumers have used telemedicine than ever before. Venture investment in telemedicine is up, and big and small players are making land grabs for their share of the market, with many rolling out virtual–first care offerings. So with these accelerants—balanced with the full return of in-person care—what’s the state of telemedicine?
To answer this question and many more, we have surveyed U.S. adults every year since 2015 to check in with consumers and their relationship to digital health. Rock Health’s Digital Health Consumer Adoption Survey (hereto referred to as the “Survey”) is a U.S. Census-matched sample of adults age 18 and over—with a distinct group of adults surveyed each year. Respondents used their personal desktop, laptop, smartphone, or tablet to complete the survey in English. In both 2020 and 2021, 7,980 U.S. adults were surveyed each year in the summer to fall timeframe; in previous years, we surveyed approximately 4,000 U.S. adults annually. For statistical analyses, we used logistic regression to determine the association between a primary predictor and outcome of interest, controlling for covariates (i.e., confounders) in multivariate regression analysis.
Before we dive in, let’s define our terms. We define telemedicine as tech-enabled modalities that enable consumers to receive medical care or advice remotely from clinicians. Telemedicine can be synchronous (a live video visit or phone call) or asynchronous (exchanging a text, email, or picture with a clinician).
The pandemic-induced demand for remote care—and the accompanying ingenuity of innovators at organizations big and small—have evolved the conventional parameters of telemedicine. Here’s how we see a few assumptions about telemedicine being replaced by new paradigms:
- Old: Telemedicine as a business model. → New: Telemedicine as a tool.
- Old: Virtual care. → New: Virtual-first care.
- Old: Telemedicine built for the masses. → New: Telemedicine built for (more) targeted care needs.
Let’s be clear: traditional telemedicine service providers are not going away anytime soon. They’ve become entrenched (and in some cases, massive) organizations that will continue to compete in an increasingly commoditized market where winning is predominantly about market share, not product differentiation. But beyond the traditional video visit, telemedicine is now embedded in many solutions as a tool to connect patients and providers. Few (if any) emerging startups today would call themselves “telemedicine companies.” Instead, telemedicine is one tool within a comprehensive offering and experience. Noom is a weight loss management company, Ro is (in part) a digital pharmacy, and LetsGetChecked is an at-home lab testing company. In these examples—and across nearly every company in the virtual care space—some modality of telemedicine is combined with other tools (e.g., remote patient tracking, at-home diagnostics, dynamic content) to engage clinicians and patients, and ultimately drive toward outcomes.
Exciting innovations around at-home diagnostics, digital biomarkers, and monitoring are making more remote care possible. However, a consumer-directed journey doesn’t operate exclusively in a virtual care model; it interacts with virtual and expansive in-person care touchpoints—in the home, physician practices, hospitals, retail clinics, urgent care, etc. Health plans, retailers, and providers alike are converging on this omnichannel experience that integrates online-to-offline (and back again) care experiences.
Telemedicine 1.0 brought in-person interactions online. And, a largely “one-size-fits-all” model met initial demand from employers and health insurers to offer solutions that could accommodate vast employee/member populations. To drive greater engagement and consistent outcomes, telemedicine tools are now increasingly being built for specific clinical issues (e.g., autoimmune disorders, reproductive health), consumer groups (e.g., LGBTQ+ community, women+1), or both (e.g., adolescent behavioral health).
As investors in startups and advisors to enterprise, it’s exciting to watch these shifts create new opportunities across the market. But, it’s also important to balance perspectives on emerging innovation with a close look at which solutions are actually reaching consumers. In other words, which people are using telemedicine? Do they like it? What are they using it for? And will they continue to use it?
Below, we share three insights from the 2021 Survey. We hope they support the work of innovators at startups, enterprises, and in the public sphere as they continue the important work of building healthcare (and virtual care) with consumers at the center.
INSIGHT #1: While the current COVID paradigm has bolstered live video to the most-used telemedicine modality, future virtual care models will increasingly integrate audio and asynchronous modalities.
2021 marks the first year in which live video was the most used telemedicine modality (among live video, live phone, text messaging, email, messaging via a health app or website, and picture or video messaging). Fifty-one percent of 2021 respondents have previously used live video telemedicine–eight percentage points higher than 2020, and 19 points higher than 2019.
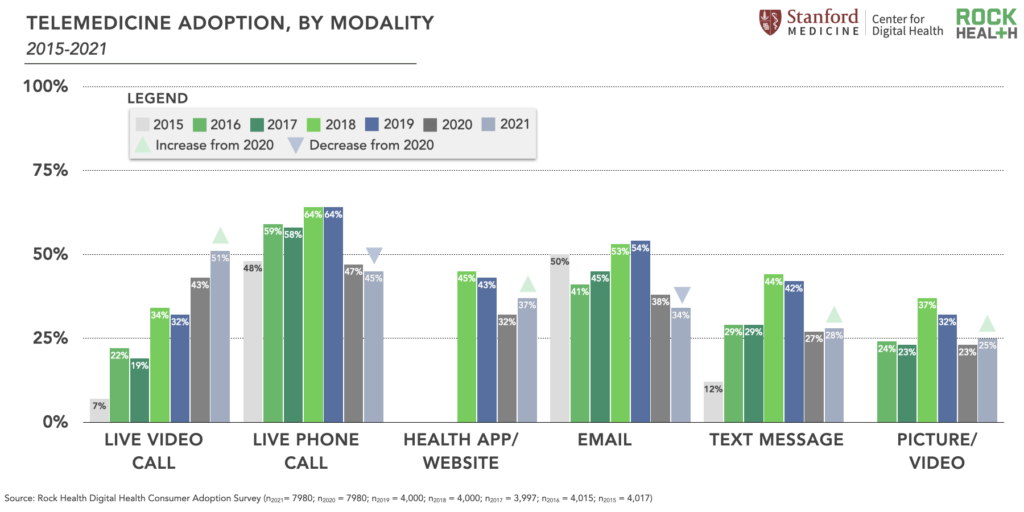
We view the rapid rise in live video adoption as a predominantly supply-driven phenomenon. Specifically, more clinicians are offering video telemedicine than ever before, in large part because of COVID-induced payment and regulatory changes to encourage said adoption. As evidence of the expanded supply, less than half (44%) of 2021 Survey respondents with an established primary care provider (PCP) reported that their PCP offered telemedicine prior to the pandemic; 23% of those respondents weren’t sure. But as of August 2021, 80% of those same respondents said their PCP offered telemedicine, with 11% not sure.2
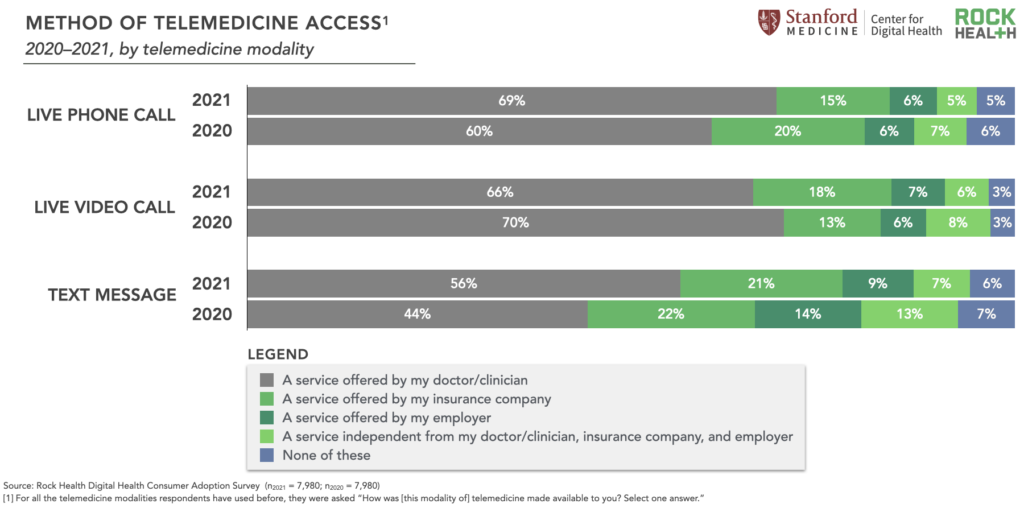
Physician adoption of live video telemedicine skyrocketed in 2020 so care delivery would not come to a screeching halt. And even with the return of in-person care, the majority of 2021 Survey respondents reported that these offerings are still widely available through their PCP. So it’s not surprising that across 2020-2021, approximately two-thirds of respondents reported accessing live video telemedicine through their clinician, as opposed to through their insurance, employer, or other service.
Implications
In healthcare, regulation and reimbursement are never fixed—and that remains true with policies surrounding the payment, security, and regulation of different telemedicine modalities. Many stakeholders are advocating for national and state-level policies that continue and expand access to telehealth services. And while CMS announced it will keep select video and audio-only services on its telehealth reimbursement list through 2023, many state-level proposed policies are still pending. While audio-only telemedicine was rarely reimbursed prior to COVID, many are now calling for it to be permanently safeguarded. Whether live video or audio-only telemedicine is reimbursed at parity and for which services will impact the degree to which providers embrace specific telemedicine modalities.
Perhaps more motivating than future reimbursement paradigms is the opportunity presented by embracing hybrid virtual-in-person models—and the threat if traditional providers don’t. Entrepreneurs, new market entrants, retail giants, and select incumbents are moving quickly to cement their strategy in a virtual-first care world. Even the biggest of players, Amazon, announced its intention to scale its virtual and house call offering, Amazon Care, to all 50 states. It is this market competition that we believe will keep all stakeholders on their toes and pointed toward offering consumer-centric, omnichannel care.
As more virtual care offerings become available (through plans, employers, retail, and direct-to-consumer channels), we expect non-video telemedicine modalities to become a common tool within emerging care models. Advocates recognize its positive impact on underserved populations. And asynchronous telemedicine modalities present a number of opportunities: enhanced clinician efficiency which enables a more scalable (and sustainable) workforce model, and a patient experience in which care is proactive and integrated into one’s life (especially considering the preferences of the Millennial “texting generation”). Just a handful of the many startups embracing asynchronous telemedicine include: K Health, BetterHelp, MindRight, and Cerebral, which use in-app provider messaging to address different needs (e.g., primary care, mental health, and urgent care), and Nurx, which uses photo sharing to enable remote assessment of skin conditions.
Amidst telehealth reimbursement uncertainty, innovators of virtual care models will need to design and test for the optimal mix of telemedicine modalities to meet the needs of the population they’re building for. Designing toward the North Star of improved outcomes at reduced costs will allow entrepreneurs to embrace business model innovation—and specifically value-based care models—regardless of the specific reimbursement codes that may or may not include specific provider-patient care interactions.
INSIGHT #2: Relative to in-person care, most consumers remain satisfied with telemedicine, though satisfaction fell from 2020’s peak.
Overall, consumers remain highly satisfied with telemedicine. In 2020, the majority of respondents (53%) reported greater satisfaction with live video telemedicine compared to prior in-person care interactions. However, in 2021, this satisfaction decreased: 43% of respondents reported greater satisfaction with live video calls compared to in-person care. A big dip, to be sure.
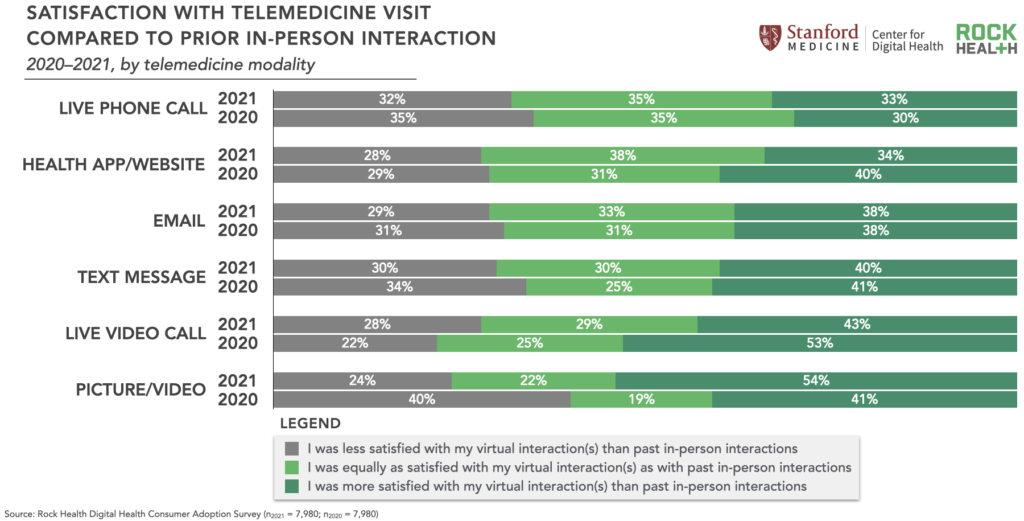
One hypothesis is that as the pandemic evolved, consumers started viewing telemedicine as an alternative to in-person care, rather than a necessary replacement. In other words, the sense of satisfaction (maybe as a barometer for gratitude) consumers felt for having the option of telemedicine in 2020 has diminished. Something similar happened with physicians: 58% of surveyed physicians in 2021 view telehealth more favorably now than they did before COVID-19, compared to 64% of physicians surveyed in 2020.
Between 2020-2021, consumers changed the way they used telemedicine, which could be another explanation for decreased satisfaction. In 2021, respondents primarily accessed live video calls for a minor illness (32%), followed by a medical emergency (20%) and chronic condition (18%). This is a departure from 2020 when telemedicine users primarily accessed live video calls for a medical emergency (33%). This shift feels welcome and is a better reflection of the strengths of (current) telemedicine capabilities, which are better suited for lower-acuity issues rather than true medical emergencies.
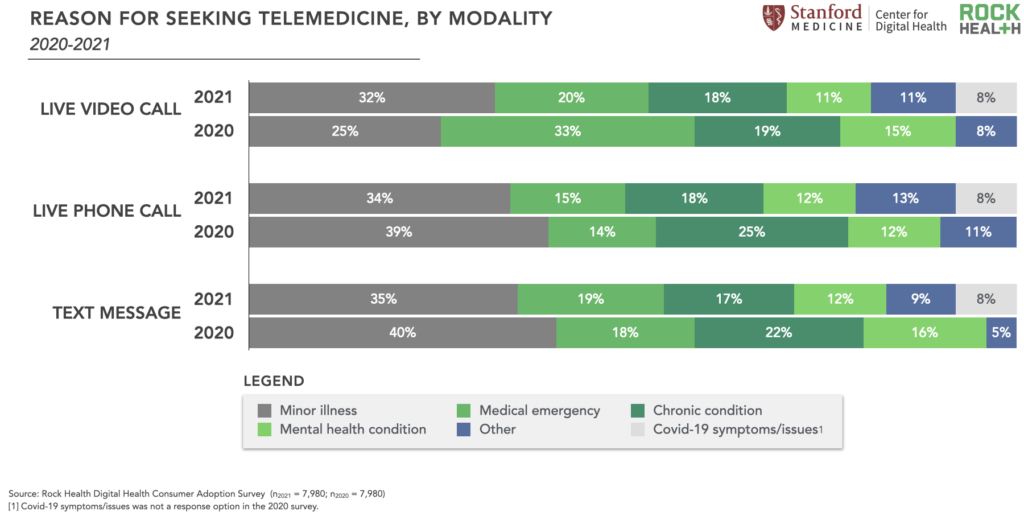
However, 2021 Survey data imply that satisfaction with telemedicine as a convenient alternative may be lower than telemedicine as a necessary access point. Seventy-seven percent of respondents who accessed live video telemedicine for a medical emergency reported higher satisfaction with those virtual interactions compared to in-person care. Satisfaction was not as pronounced for other use cases: 37% of respondents who used live video telemedicine for a minor illness reported higher satisfaction compared to in-person care, and 28% of those using live video telemedicine for a chronic condition.
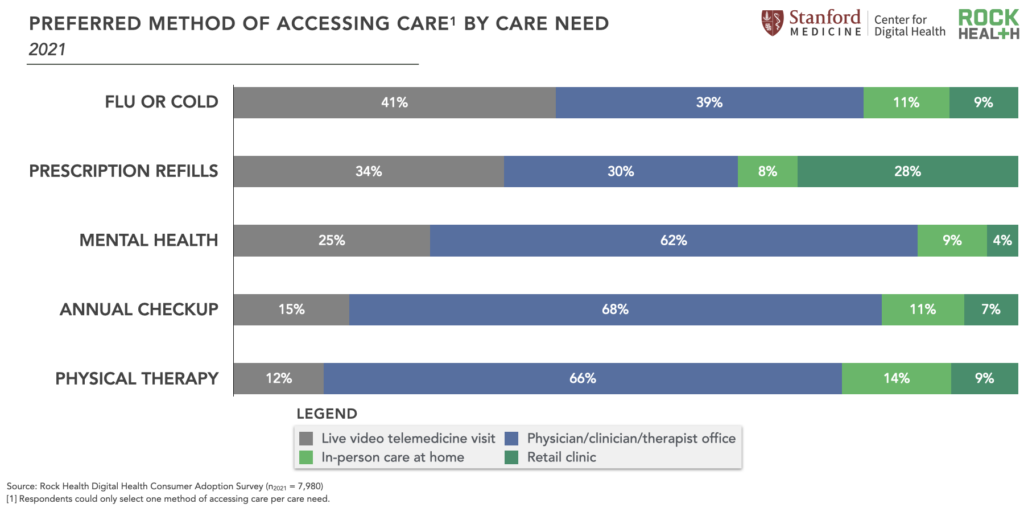
With more and varied telemedicine options available, we are moving from evaluating “telemedicine satisfaction” as a monolith to understanding consumer preferences within specific contexts. Just like in-person care, people will like (and dislike) telemedicine experiences based on a wide range of factors—the convenience and accessibility of the interaction, the “webside manner” of the clinician, whether their need was fulfilled, cost, etc. And, consumers will compare these experiences to their in-person alternatives. As we push to understand the stratification of consumer telemedicine preferences—and its implications for builders of such solutions—here’s a start: more 2021 Survey respondents reported a preference for receiving flu/cold care and prescription refills through live video visits compared to any other discrete option, including visiting a clinician’s office, receiving in-person care at home, or going to a retail clinic. Comparatively, the majority of respondents prefer to access physical therapy, annual checkups, and mental healthcare through a clinician’s office compared to any other access point, including live video visits.
Implications
Even with recent reductions in telemedicine satisfaction, 73% of previous telemedicine users expect to use it at the same rate or more in the future3. We believe two factors will impact telemedicine satisfaction and sustained adoption moving forward: personalization and fulfillment.
Personalization is key. Our hope is innovators will continue to build with and alongside specific populations with unique and distinct care needs, bucking a one-size-fits-all approach. We’re excited to see continued specialization in digital healthcare for needs and populations that would benefit from more tailored care and navigation services.
Fulfillment is another driver of satisfaction. We’re big believers that telemedicine is only valuable insofar as it guides the patient efficiently from healthcare need to fulfillment of said need. The consumer experience should enable ease, speed, and personalization of care navigation all the way through care delivery. Moving forward, we’re excited about solutions that quickly triage the patient’s need, assign the appropriate care setting (in-person or virtual), help patients navigate to the best option, fulfill the need, and provide accessible payment, data-sharing, and ongoing management services. Companies that can bring together assets (via ownership or partnership) along this care journey—triage, virtual and in-person care, diagnostics, labs, medication delivery—are poised to win with consumers.
INSIGHT #3: Telemedicine adoption trends suggest inequities in access—younger consumers with higher incomes and education levels continue to use telemedicine at the highest rates.
Digital inequities and distrust widely permeate the healthcare industry, and despite its promise, digital health may leave some patients behind by exacerbating existing gaps related to internet and tech access, device ownership, and digital literacy.
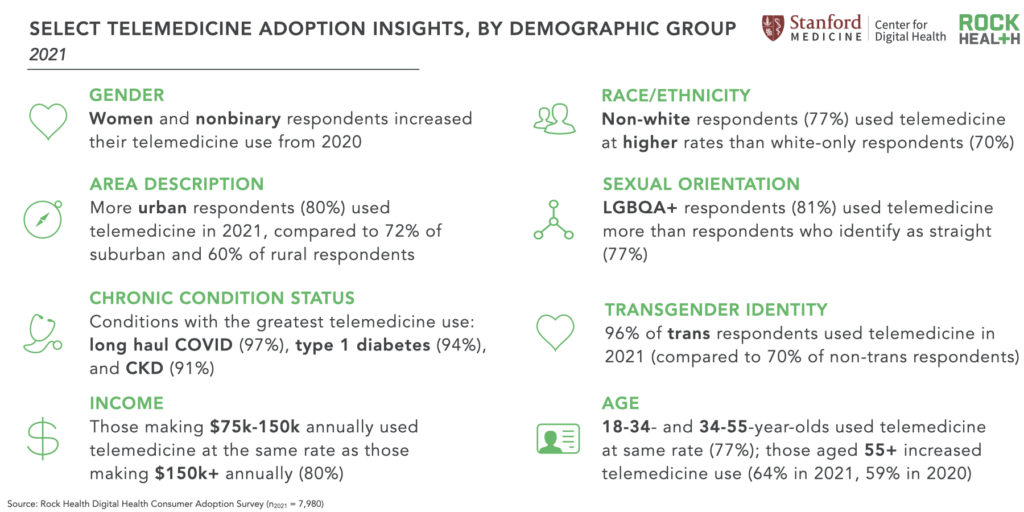
In line with previous years, the most likely users of telemedicine in 2021 were higher-income earners4, younger respondents (aged 18-44)5, those with chronic conditions6, and respondents with advanced educational degrees.7 In 2021, women were more likely to use telemedicine compared to men respondents, a change from 2020.8 And, in 2021, race/ethnicity was associated with telemedicine use: non-white respondents were significantly more likely to use telemedicine than those who identify as white-only.9 Seventy percent of white-only respondents in 2021 reported telemedicine use, compared to 87% of Hawaiian Native and/or Pacific Islander respondents, 79% of Black respondents, 79% of American Indian and/or Alaska Native respondents, 78% of Asian respondents, and 73% of Hispanic respondents.10 Collectively, respondents that identify as non-white increased their telemedicine use by eight percentage points from 2020.
According to a 2021 Pew study, Black and Hispanic adults are less likely than white adults to own a desktop/laptop computer or have high-speed internet at home.11 Since our Survey was completed in English via the internet, the methodology may mean certain groups are underrepresented. However, our finding aligns with a 2020 Pew study which found Black, Hispanic, and other non-white adults were more likely than white adults to use telemedicine. The study suggests that systemic racism contributing to healthcare disparities raised the need for these services, particularly among Black patients, during the pandemic.12
Respondents who reported using telemedicine the most (younger, those with higher income, or those with higher education) also reported the highest rates of expected continued or increased telemedicine use. The anticipated use of telemedicine was less common among older respondents, those with lower incomes, and among respondents with lower educational attainment. Unfortunately, these data imply that groups with historically low access to healthcare are disproportionately precluded from the benefits of telemedicine: increased convenience, better access to providers, and, in some cases, reduced out-of-pocket expenses.
To learn more about how demographic factors (e.g., gender, age, insurance status) impact telemedicine adoption, reach out to us! Rock Health has seven years of trended consumer adoption data.
Twenty-eight percent of 2021 respondents reported no prior use of telemedicine via any modality. The following groups were least likely to have used telemedicine before13: adults 55+, those making less than $35k annually, rural respondents, those taking zero prescriptions, and those without insurance.14
Of note, rural respondents were one of the few groups whose telemedicine adoption remained stagnant from 2020 to 2021. Across both years, 40% of rural respondents reported no use of telemedicine. And compared to their urban counterparts, rural respondents were significantly less likely to use telemedicine.15 Mimicking adoption broadly, rural respondents reported that many of their PCPs started offering telemedicine during the pandemic, though still at lower rates than other areas: 72% of rural respondents reported their PCPs offered telemedicine in 2021, compared to 80% of suburban and 86% of urban respondents. However, 9% of 2021 rural respondents that never accessed telemedicine reported poor cellular or broadband connectivity as a barrier to using telemedicine compared to 4% of non-rural respondents. And, compared to urban respondents, rural respondents are less likely to be more satisfied with live video calls compared to previous in-person care interactions.16
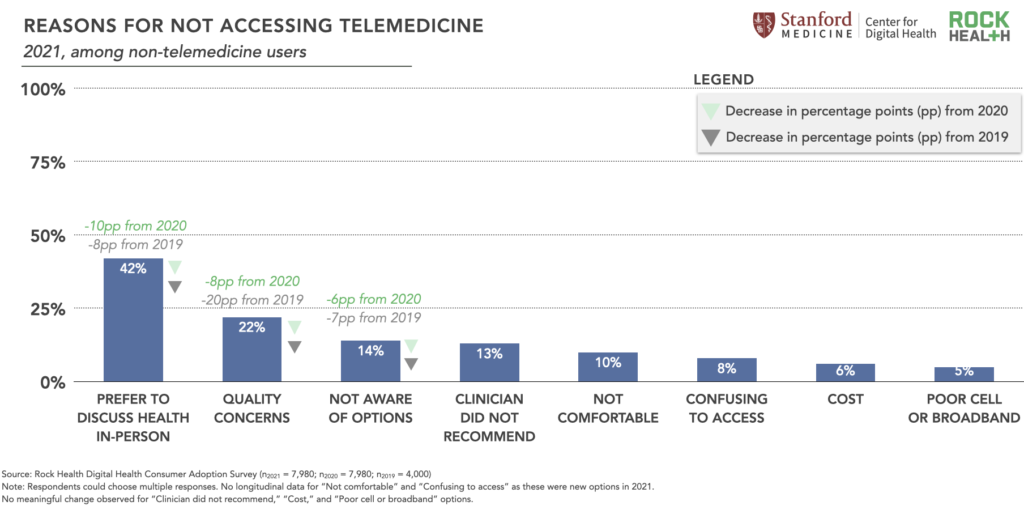
As shown in the figure below, 2021 Survey respondents who have never used telemedicine reported their primary reasons for non-use as: preference to discuss health in-person, concerns over quality of care, and not being aware of telemedicine as an option. While preferring to discuss health in-person remains the primary reason, it’s worth noting that this response decreased by 10 percentage points compared to 2020.
Implications
Through this data, we hope to support digital health innovators as they seek to deeply understand the population they want to build for, and what factors may be driving (or preventing) that population’s digital health adoption.
By building alongside communities and learning their goals and contexts, companies are increasingly addressing the telemedicine utilization gap. For example, Ginger newly offers Spanish-language services, SilverCloud tailors solutions for medically underserved populations, and Pomelo Care and Mahmee provide equitable maternal and pregnancy care outcomes especially for Black individuals. Included Health is a virtual-first platform with offerings tailored to underrepresented communities such as LGBTQ+ individuals and people of color. This, combined with the larger policy pushes necessary to overcome health disparities, is a move toward true (tele)health for all.
Telemedicine’s path forward
In 2020, we offered the analogy of a pendulum to describe the rise in virtual care use, put into motion by the pandemic. The 2021 Survey gives us new data to understand where that pendulum may land over the next few years, with virtual and in-person care options widely available. The data points to continued use of virtual care by clinicians and consumers alike. Satisfaction for telemedicine remains high, though nuanced preferences highlight the opportunity for innovators to compete on experience and outcomes.
We expect virtual-first care models to proliferate, with novel and varied uses of all telemedicine modalities. This untethering from the live video visit will enable models that are more scalable, cost-effective, accessible, and ultimately, more equitable. With innovators focused on creating value through personalized virtual care experiences and need fulfillment, it’s clear there is a promising path forward for telemedicine-enabled care.
Diving into seven years of consumer insights
Want to dig even further into this longitudinal data? Reach out to advisory@rockhealth.com to learn more about the Rock Health Enterprise Membership and how we can help you explore questions like:
- How are consumers using wearables differently during COVID-19?
- What factors influence a consumers’ willingness to share their healthcare data?
- What specific types of data (e.g., lab test results, COVID-19 vaccination status) are consumers more (or less) willing to share with stakeholders such as providers, health insurers, and employers?
Don’t miss our next piece on 2021 consumer adoption of digital health—subscribe to the Rock Weekly.
Footnotes
- We use the term “women+ health” to describe the space to encompass the full spectrum of health needs experienced by cisgender women, as well as others whose health needs relate to those of cisgender women but may identify as transgender or non-binary.
- Seventy-six percent of 2021 Survey respondents (6,097 of 7,980) reported having an established primary care practice or clinician that they see annually.
- We excluded ~3% of responses given inconsistent answers among respondents.
- Respondents with annual incomes of $150,000 to $199,999 had significantly higher odds of using telemedicine in univariate (OR: 3.51; CI: 2.74-4.50; p<0.001) and covariate-adjusted regression analysis (OR: 2.09; CI:1.56-2.80; p<0.001) compared to lower-income groups. Likewise, those with an annual income of over $200,000 had significantly higher odds of using telemedicine in univariate (OR: 2.16; CI:1.76-2.63; p<0.001) and covariate-adjusted (OR: 1.36; CI:1.05-1.75; p= 0.018) regression analysis.
- Older respondents were significantly less likely to use telemedicine compared to younger respondents aged 18-44 (55-64 years: OR:0.38; CI:0.30-0.47; p<0.001; 65-74 years: OR:0.26; CI:0.20-0.34; p<0.001; 75+ years: OR:0.22; CI:0.16-0.29; p<0.001).
- Respondents with at least one chronic condition had significantly greater odds of telemedicine use compared to those without a chronic condition (OR:3.68; CI:3.20-4.12; p<0.001).
- Compared to high school or less than high school graduates, respondents with higher educational attainment had significantly greater odds of telemedicine usage (Master’s degree OR: 2.38; CI:1.64-3.46; p<0.001; Ph.D. degree OR: 2.78; CI:1.51-5.09; p=0.001; Graduate or professional degree OR: 2.48; CI:1.60-3.84; p<0.001).
- Men were less likely to use telemedicine compared to women in a covariate-adjusted regression analysis. Non-binary had lower odds of using telemedicine but not significantly (men OR: 0.85; CI: 0.76-0.94; p=0.004; non-binary OR: 0.95; CI: 0.52-1.73; p=0.86).
- Seventy-seven percent of non-white respondents in 2021 reported telemedicine use compared to 70% of white-only respondents. Non-white respondents compared to white respondents had significantly greater odds of using telemedicine (OR:1.19; CI:1.05-1.36; p=0.007).
- The Survey asked respondents to note which races/ethnicities they identify with, and respondents could choose multiple responses. These were the N sizes for each race/ethnicity in the 2021 Survey: Hawaiian Native and/or Pacific Islander (n=92), Black (n=1,080), American Indian and/or Alaska Native (n=219), Asian (n=431), Hispanic (n=1,354), and white-only (n=4,961).
- The Pew Research Center’s 2021 survey found that 80% of surveyed white adults reported owning a desktop or laptop computer, compared with 69% of Black adults and 67% of Hispanic adults. In addition, 80% of white adults reported having a broadband connection at home, while smaller shares of Black and Hispanic adults said the same (71% and 65%, respectively). They note these gaps are present across several Pew surveys.
- The Pew Research Center survey measured telehealth use during the pandemic by asking whether respondents (n=10,624) “used the internet or e-mail to connect with doctors or other medical professionals as a result of the coronavirus outbreak.”
- These groups all had lower odds of telemedicine use in regression analysis (as shown in previous footnotes).
- Compared to respondents having insurance through a current or former employer or union, those who reported not having health insurance coverage had the lowest odds of using telemedicine in covariate adjusted regression analysis (OR: 0.29; CI:0.23-0.37; p<0.001).
- Suburban and rural respondents compared to urban have significantly lower odds of telemedicine use (suburban: OR:0.76; CI:0.67-0.87; p<0.001; rural: OR:0.56; CI:0.48-0.65; p<0.001).
- Urban (57.96%) more than suburban (32.3%) and rural (9.75%) respondents reported more satisfaction with live video interaction than past in-person interactions (P<0.001).


